肝细胞癌新辅助治疗的现状与展望
DOI: 10.3969/j.issn.1001-5256.2023.11.027
-
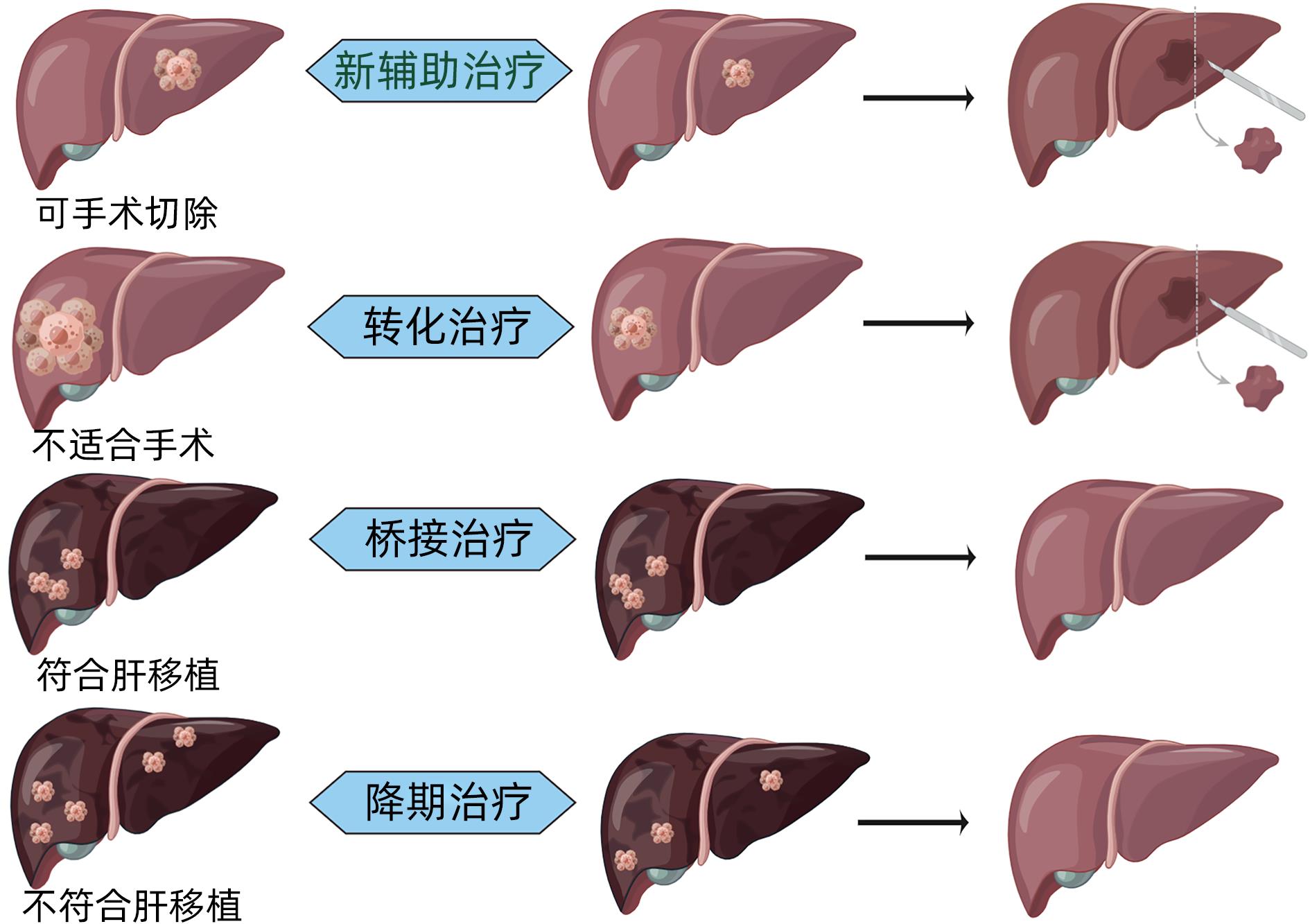
摘要: 肝细胞癌(HCC)是癌症相关死亡的主要原因,手术切除是重要的根治性治疗手段,但术后高复发率仍是当前亟待解决的问题。新辅助治疗可降低术后高复发率,既往因缺乏有效的治疗手段,肝癌的新辅助治疗临床获益甚微。当前基于免疫检查点抑制剂的联合治疗,因其高有效率改变了晚期HCC患者的治疗格局。这促使研究者重新审视HCC的新辅助治疗策略,期望通过新辅助治疗能提供新的机会,降低术后复发率,提高治疗后的生存率。本文就HCC新辅助治疗的现状和前景及一些热点问题进行探讨,以期为其治疗提供更多思路。Abstract: Hepatocellular carcinoma (HCC) is a major cause of cancer-related death, and surgical resection remains an important method for radical treatment, but it is urgently needed to solve the problem of high postoperative recurrence rate. Neoadjuvant therapy can reduce the high recurrence rate after surgery, and there are little benefits from neoadjuvant therapy for HCC due to a lack of effective treatment methods in the past. At present, combination therapy based on immune checkpoint inhibitors has a relatively high response rate and has thus changed the treatment landscape for patients with advanced HCC. This urges investigators to reexamine the neoadjuvant treatment strategies for HCC, and it is expected that neoadjuvant therapy can provide new opportunities, reduce the postoperative recurrence rate, and improve the survival rate after treatment. This article discusses the current status and prospects of neoadjuvant therapy for HCC and related hot topics, so as to provide more ideas for exploring neoadjuvant therapy for HCC.
-
Key words:
- Carcinoma, Hepatocellular /
- Neoadjuvant Therapy /
- Treatment Outcome
-
表 1 肝癌局部治疗模式的技术优势对比
Table 1. Comparison of technical advantages of locoregional therapy for HCC
策略 技术 应用和优势 不良反应 TACE c-TACE/d-TACE 转化、桥接治疗 栓塞综合征、肝功能损伤 TARE 90Y放射微球 合并PVTT/增加对侧肝叶体积 栓塞综合征、肝功能损伤、放射性肝损害 放疗 3-DCRT/SBRT/IMRT 合并PVTT 放射性肝损害 HAIC FOLFOX 合并PVTT/降低微血管侵犯 疼痛/骨髓抑制/消化道症状 注:3-DCRT,三维适形放疗;SBRT,立体定向放疗;IMRT,调强放疗。不同研究之间结果不可直接对比。 表 2 肝癌新辅助在研的局部治疗方案
Table 2. Selected studies on the use of neoadjuvant locoregional therapy
治疗方案 方法 纳入人群 主要研究终点 次要研究终点 NCT04025437 放疗 Ⅰ型PVTT 总生存期 RFS NCT04587739 SBRT 3~8 cm单病灶 退出率 放射毒性、总生存期、DFS、手术情况 NCT03469479 HAIC 超米兰可切除 总生存期 RFS、不良反应 NCT0385193 HAIC 超米兰BCLC A/B 总生存期 RFS、PFS、复发率 NCT03368651 HAIC PVTT 总生存期 RFS、PFS、复发率 NCT04181931 HAIC+TACE PVTT PFS 总生存期 NCT04424043 HAIC+TACE BCLC B PFS 总生存期 NCT0477794 HAIC+TACE BCLC A高危 PFS 总生存期 -
[1] SUNG H, FERLAY J, SIEGEL RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71( 3): 209- 249. DOI: 10.3322/caac.21660. [2] PARK JW, CHEN M, COLOMBO M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study[J]. Liver Int, 2015, 35( 9): 2155- 2166. DOI: 10.1111/liv.12818. [3] KORDE LA, SOMERFIELD MR, CAREY LA, et al. Neoadjuvant chemotherapy, endocrine therapy, and targeted therapy for breast cancer: ASCO guideline[J]. J Clin Oncol, 2021, 39( 13): 1485- 1505. DOI: 10.1200/JCO.20.03399. [4] HANK T, BÜCHLER MW, NEOPTOLEMOS JP. Neoadjuvant chemotherapy in pancreatic cancer[J]. JAMA Surg, 2021, 156( 4): 397- 397. DOI: 10.1001/jamasurg.2020.6273. [5] ROSEN G, MARCOVE R C, CAPARROS B, et al. Primary osteogenic sarcoma. The rationale for preoperative chemotherapy and delayed surgery[J]. Cancer, 1979, 43( 6): 2163- 2177. DOI: 3.0.co;2-s">10.1002/1097-0142(197906)43:6<2163::aid-cncr2820430602>3.0.co;2-s. [6] FREI E 3rd. Clinical cancer research: an embattled species[J]. Cancer, 1982, 50( 10): 1979- 1992. DOI: 3.0.co;2-d">10.1002/1097-0142(19821115)50:10<1979::aid-cncr2820501002>3.0.co;2-d. [7] TRIMBLE EL, UNGERLEIDER RS, ABRAMS JA, et al. Neoadjuvant therapy in cancer treatment[J]. Cancer, 1993, 72( 11 Suppl): 3515- 3524. DOI: 10.1002/1097-0142(19931201)72:11 +<3515::aid-cncr2820721619>3. 0.co;2-a. [8] HWANG TL, CHEN MF, LEE TY, et al. Resection of hepatocellular carcinoma after transcatheter arterial embolization. Reevaluation of the advantages and disadvantages of preoperative embolization[J]. Arch Surg, 1987, 122( 7): 756- 759. DOI: 10.1001/archsurg.1987.01400190022004. [9] General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009.国家卫生健康委办公厅. 原发性肝癌诊疗指南(2022年版)[J]. 临床肝胆病杂志, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. [10] ZHOU H, SONG T. Conversion therapy and maintenance therapy for primary hepatocellular carcinoma[J]. Biosci Trends, 2021, 15( 3): 155- 160. DOI: 10.5582/bst.2021.01091. [11] POON RT, FAN ST, NG IO, et al. Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma[J]. Cancer, 2000, 89( 3): 500- 507. [12] TSILIMIGRAS DI, BAGANTE F, MORIS D, et al. Recurrence patterns and outcomes after resection of hepatocellular carcinoma within and beyond the barcelona clinic liver cancer criteria[J]. Ann Surg Oncol, 2020, 27( 7): 2321- 2331. DOI: 10.1245/s10434-020-08452-3. [13] ZHAO H, HUA Y, DAI T, et al. Development and validation of a novel predictive scoring model for microvascular invasion in patients with hepatocellular carcinoma[J]. Eur J Radiol, 2017, 88: 32- 40. DOI: 10.1016/j.ejrad.2016.12.030. [14] von FELDEN J, HEIM D, SCHULZE K, et al. High expression of micro RNA-135A in hepatocellular carcinoma is associated with recurrence within 12 months after resection[J]. BMC Cancer, 2017, 17( 1): 60. DOI: 10.1186/s12885-017-3053-7. [15] LIU T, TAN J, WU M, et al. High-affinity neoantigens correlate with better prognosis and trigger potent antihepatocellular carcinoma(HCC) activity by activating CD39+ CD8+ T cells[J]. Gut, 2021, 70( 10): 1965- 1977. DOI: 10.1136/gutjnl-2020-322196. [16] HARDING JJ, NANDAKUMAR S, ARMENIA J, et al. Prospective genotyping of hepatocellular carcinoma: clinical implications of next-generation sequencing for matching patients to targeted and immune therapies[J]. Clin Cancer Res, 2019, 25( 7): 2116- 2126. DOI: 10.1158/1078-0432.CCR-18-2293. [17] HORWITZ E, STEIN I, ANDREOZZI M, et al. Human and mouse VEGFA-amplified hepatocellular carcinomas are highly sensitive to sorafenib treatment[J]. Cancer Discov, 2014, 4( 6): 730- 743. DOI: 10.1158/2159-8290.CD-13-0782. [18] ZHANG Z, LIU Q, HE J, et al. The effect of preoperative transcatheter hepatic arterial chemoembolization on disease-free survival after hepatectomy for hepatocellular carcinoma[J]. Cancer, 2000, 89( 12): 2606- 2612. [19] GERUNDA GE, NERI D, MERENDA R, et al. Role of transarterial chemoembolization before liver resection for hepatocarcinoma[J]. Liver Transpl, 2000, 6( 5): 619- 626. DOI: 10.1053/jlts.2000.8312. [20] CHUA TC, LIAUW W, SAXENA A, et al. Systematic review of neoadjuvant transarterial chemoembolization for resectable hepatocellular carcinoma[J]. Liver Int, 2010, 30( 2): 166- 174. DOI: 10.1111/j.1478-3231.2009.02166.x. [21] QADAN M, FONG ZV, DELMAN AM, et al. Review of use of Y90 as a bridge to liver resection and transplantation in hepatocellular carcinoma[J]. J Gastrointest Surg, 2021, 25: 2690- 2699. DOI: 10.1007/s11605-021-05095-x. [22] SALEM R, JOHNSON GE, KIM E, et al. Yttrium‐90 radioembolization for the treatment of solitary, unresectable HCC: the LEGACY study[J]. Hepatology, 2021, 74( 5): 2342- 2352. DOI: 10.1002/hep.31819. [23] KOKABI N, CAMACHO JC, XING M, et al. Open‐label prospective study of the safety and efficacy of glass‐based yttrium 90 radioembolization for infiltrative hepatocellular carcinoma with portal vein thrombosis[J]. Cancer, 2015, 121( 13): 2164- 2174. DOI: 10.1002/cncr.29275. [24] WEI X, JIANG Y, ZHANG X, et al. Neoadjuvant three-dimensional conformal radiotherapy for resectable hepatocellular carcinoma with portal vein tumor thrombus: a randomized, open-label, multicenter controlled study[J]. J Clin Oncol, 2019, 37( 24): 2141. DOI: 10.1200/JCO.18.02184. [25] KAMIYAMA T, NAKANISHI K, YOKOO H, et al. Efficacy of preoperative radiotherapy to portal vein tumor thrombus in the main trunk or first branch in patients with hepatocellular carcinoma[J]. Int J Clin Oncol, 2007, 12( 5): 363- 368. DOI: 10.1007/s10147-007-0701-y. [26] LI Q J, HE M K, CHEN H W, et al. Hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin versus transarterial chemoembolization for large hepatocellular carcinoma: a randomized phase Ⅲ trial[J]. J Clin Oncol, 2022, 40( 2): 150- 160. DOI: 10.1200/JCO.21.00608. [27] HE MK, LE Y, LI QJ, et al. Hepatic artery infusion chemotherapy using mFOLFOX versus transarterial chemoembolization for massive unresectable hepatocellular carcinoma: a prospective non-randomized study[J]. Chin J Cancer, 2017, 36( 1): 83. DOI: 10.1186/s40880-017-0251-2. [28] LYU N, WANG X, LI J B, et al. Arterial chemotherapy of oxaliplatin plus fluorouracil versus sorafenib in advanced hepatocellular carcinoma: a biomolecular exploratory, randomized, phase Ⅲ trial(FOHAIC-1)[J]. J Clin Oncol, 2022, 40( 5): 468- 480. DOI: 10.1200/JCO.21.01963. [29] HUANG J, HUANG W, ZHAN M, et al. Drug-eluting bead transarterial chemoembolization combined with FOLFOX-based hepatic arterial infusion chemotherapy for large or huge hepatocellular carcinoma[J]. J Hepatocell Carcinoma, 2021, 8: 1445- 1458. DOI: 10.2147/JHC.S339379. [30] BYUN HK, KIM HJ, IM YR, et al. Dose escalation by intensity modulated radiotherapy in liver-directed concurrent chemoradiotherapy for locally advanced BCLC stage C hepatocellular carcinoma[J]. Radiother Oncol, 2019, 133: 1- 8. DOI: 10.1016/j.radonc.2018.12.025. [31] BARBIER L, FUKS D, PESSAUX P, et al. Safety of liver resection for hepatocellular carcinoma after sorafenib therapy: a multicenter case-matched study[J]. Ann Surg Oncol, 2013, 20( 11): 3603- 3609. DOI: 10.1245/s10434-013-3029-z. [32] KUDO M, FINN R S, QIN S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial[J]. Lancet, 2018, 391( 10126): 1163- 1173. DOI: 10.1016/S0140-6736(18)30207-1. [33] TADA M, ICHIDA A, ARITA J, et al. Multicenter prospective study to evaluate the efficacy of lenvatinib to achieve conversion surgery for initially unresectable hepatocellular carcinoma: LENS-HCC trial[J]. J Clin Oncol, 2022, 40( 4): 458. DOI: 10.1200/JCO.2022.40.4_suppl.458. [34] YANG XR, SUN HC, XIE Q, et al. Chinese expert guidance on overall application of lenvatinib in hepatocellular carcinoma[J]. Chin J Dig Surg, 2023, 22( 2): 167- 180. DOI: 10.3760/cma.j.cn115610-20230201-00035.杨欣荣, 孙惠川, 谢青, 等. 仑伐替尼肝癌全病程应用中国专家指导意见[J]. 中华消化外科杂志, 2023, 22( 2): 167- 180. DOI: 10.3760/cma.j.cn115610-20230201-00035. [35] LIN YY, TAN CT, CHEN CW, et al. Immunomodulatory effects of current targeted therapies on hepatocellular carcinoma: implication for the future of immunotherapy[J]. Semin Liver Dis, 2018, 38( 4): 379- 388. DOI: 10.1055/s-0038-1673621. [36] LIANG J, LI L. Progress and consideration of immunotherapy strategy for hepatocellular carcinoma[J]. Chin J Dig Surg, 2021, 20( 2): 184- 190. DOI: 10.3760/cma.j.cn115610-20201228-00809.梁军, 李丽. 肝癌免疫治疗策略的进展与思考[J]. 中华消化外科杂志, 2021, 20( 2): 184- 190. DOI: 10.3760/cma.j.cn115610-20201228-00809. [37] HO WJ, ZHU Q, DURHAM J, et al. Neoadjuvant cabozantinib and nivolumab converts locally advanced HCC into resectable disease with enhanced antitumor immunity[J]. Nat Cancer, 2021, 2( 9): 891- 903. DOI: 10.1038/s43018-021-00234-4. [38] LIU J, BLAKE SJ, YONG MC, et al. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease[J]. Cancer Discov, 2016, 6( 12): 1382- 1399. DOI: 10.1158/2159-8290.CD-16-0577. [39] MARRON TU, FIEL MI, HAMON P, et al. Neoadjuvant cemiplimab for resectable hepatocellular carcinoma: a single-arm, open-label, phase 2 trial[J]. Lancet Gastroenterol Hepato, 2022, 7( 3): 219- 229. DOI: 10.1016/S2468-1253(21)00385-X. [40] KASEB AO, HASANOV E, CAO H, et al. Perioperative nivolumab monotherapy versus nivolumab plus ipilimumab in resectable hepatocellular carcinoma: a randomised, open-label, phase 2 trial[J]. Lancet Gastroenterol Hepatol, 2022, 7( 3): 208- 218. DOI: 10.1016/S2468-1253(21)00427-1. [41] RAHMA OE, HODI FS. The intersection between tumor angiogenesis and immune suppression[J]. Clin Cancer Res, 2019, 25( 18): 5449- 5457. DOI: 10.1158/1078-0432.CCR-18-1543. [42] ZHANG N, LIU XL, XU ZQ, et al. Research progress in relationship between tumor anti-angiogenesis and immunotherapy[J]. J Jilin Univ(Medicine Edition), 2021, 47( 4): 1056- 1063. DOI: 10.13481/j.1671-587X.20210434.张娜, 刘相良, 徐志强, 等. 肿瘤抗血管生成及其与免疫治疗关系的研究进展[J]. 吉林大学学报(医学版), 2021, 47( 4): 1056- 1063. DOI: 10.13481/j.1671-587X.20210434. [43] XIA Y, WANG P, PU L, et al. Preliminary efficacy and safety of perioperative treatment of camrelizumab combined with apatinib in resectable hepatocellular carcinoma(HCC): A prospective phase Ⅱ study[J]. J Clin Oncol, 2021, 39( 15_Suppl): 4082. DOI: 10.1200/JCO.2021.39.15_suppl.4082. [44] XU L, ZHANG Y, WANG X, et al. Transarterial infusion chemotherapy(TAI) combined with Sintilimab in locally advanced, potentially resectable hepatocellular carcinoma(HCC)[J]. J Clin Oncol, 2020, 38( 15_Suppl): e16593. DOI: 10.1200/JCO.2020.38.15_suppl.e16593. [45] LLOVET JM, VILLANUEVA A, MARRERO JA, et al. Trial design and endpoints in hepatocellular carcinoma: AASLD consensus conference[J]. Hepatology, 2021, 73: 158- 191. DOI: 10.1002/hep.31327. [46] KHAN KA, KERBEL RS. Improving immunotherapy outcomes with anti-angiogenic treatments and vice versa[J]. Nat Rev Clin Oncol, 2018, 15( 5): 310- 324. DOI: 10.1038/nrclinonc.2018.9. [47] COTTRELL TR, THOMPSON ED, FORDE PM, et al. Pathologic features of response to neoadjuvant anti-PD-1 in resected non-small-cell lung carcinoma: a proposal for quantitative immune-related pathologic response criteria(irPRC)[J]. Ann Oncol, 2018, 29( 8): 1853- 1860. DOI: 10.1093/annonc/mdy218. [48] SASAKI A, IWASHITA Y, SHIBATA K, et al. Preoperative transcatheter arterial chemoembolization reduces long-term survival rate after hepatic resection for resectable hepatocellular carcinoma[J]. Eur J Surg Oncol, 2006, 32( 7): 773- 779. DOI: 10.1016/j.ejso.2006.04.002. [49] FANG P, HU JH, CHENG ZG, et al. Efficacy and safety of bevacizumab for the treatment of advanced hepatocellular carcinoma: a systematic review of phase Ⅱ trials[J]. PLoS One, 2012, 7( 12): e49717. DOI: 10.1371/journal.pone.0049717. [50] BRUIX J, TAKAYAMA T, MAZZAFERRO V, et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation(STORM): a phase 3, randomised, double-blind, placebo-controlled trial[J]. Lancet Oncol, 2015, 16( 13): 1344- 1354. DOI: 10.1016/S1470-2045(15)00198-9. [51] SUN C, LI B, LI L, et al. Effect of Huaier granules on patients with middle and advanced liver cancer[J]. J Changchun Univ Chin Med, 2022, 38( 10): 1130- 1133. DOI: 10.13463/j.cnki.cczyy.2022.10.016.孙川, 李宾, 李磊, 等. 槐耳颗粒治疗中晚期肝癌[J]. 长春中医药大学学报, 2022, 38( 10): 1130- 1133. DOI: 10.13463/j.cnki.cczyy.2022.10.016. [52] WANG Z, REN Z, CHEN Y, et al. Adjuvant transarterial chemoembolization for hbv-related hepatocellular carcinoma after resection: a randomized controlled studyadjuvant TACE for HCC after resection[J]. Clin Cancer Res, 2018, 24( 9): 2074- 2081. DOI: 10.1158/1078-0432.CCR-17-2899. [53] CHEN Q, SHU C, LAURENCE AD, et al. Effect of Huaier granule on recurrence after curative resection of HCC: a multicentre, randomised clinical trial[J]. Gut, 2018, 67( 11): 2006- 2016. DOI: 10.1136/gutjnl-2018-315983. [54] FENG M, TANG C, FENG W, et al. Hepatic artery-infusion chemotherapy improved survival of hepatocellular carcinoma after radical hepatectomy[J]. Onco Targets Ther, 2017, 10: 3001- 3005. DOI: 10.2147/OTT.S136806. [55] KUANG M. Advances in neoadjuvant therapy for hepatocellular carcinoma[J]. Chin J Dig Surg, 2023, 22( 2): 202- 208. DOI: 10.3760/cma.j.cn115610-20221203-00728.匡铭. 肝细胞癌新辅助治疗研究进展[J]. 中华消化外科杂志, 2023, 22( 2): 202- 208. DOI: 10.3760/cma.j.cn115610-20221203-00728. -



 PDF下载 ( 751 KB)
PDF下载 ( 751 KB)

 下载:
下载:


