不同指南诊断标准对人工肝治疗慢加急性肝衰竭患者短期预后的影响
DOI: 10.3969/j.issn.1001-5256.2023.11.017
The influence of diagnostic criteria of different guidelines on short-term prognosis of artificial liver therapy for acute-on-chronic liver failure
-
摘要:
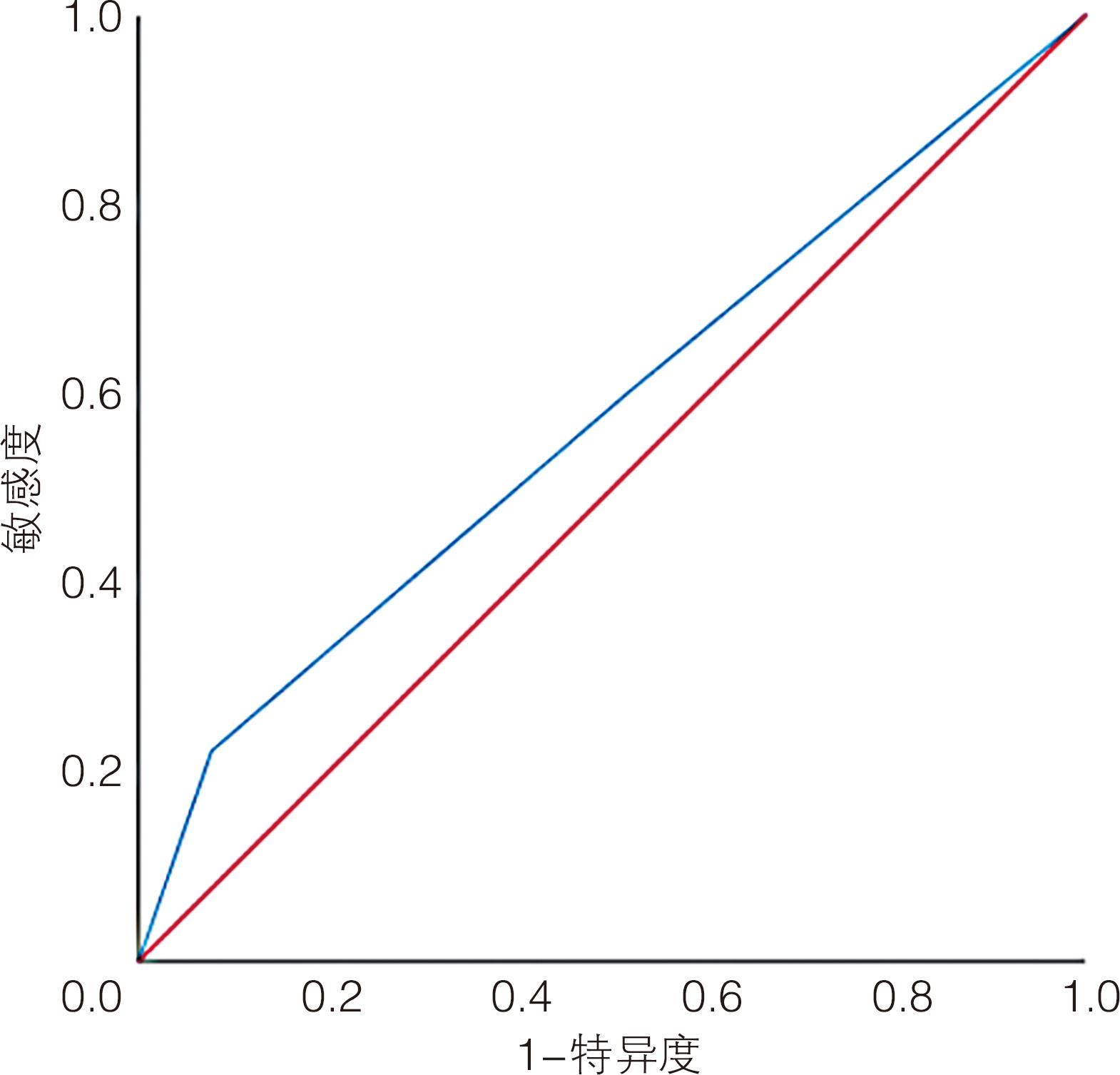
目的 探讨不同诊断标准对慢加急性肝衰竭患者短期预后的影响。 方法 纳入2018年1月—2022年1月昆明医科大学第二附属医院消化内科住院的115例慢加急性肝衰竭患者,均采用内科联合人工肝治疗。根据指南将患者分为CMA指南组(中华医学会肝衰竭诊治指南)(n=100)、APASL指南组(亚太肝病学会共识)(n=94)和EASL指南组(欧洲肝病学会标准)(n=36),随访末次人工肝治疗后90 d生存情况。计量资料组间比较采用单因素方差分析,计数资料组间比较采用χ2检验。采用受试者工作特征曲线(ROC曲线)比较上述3个指南90 d病死率的差异以及对死亡风险的预测价值。 结果 CMA指南组90 d病死率为50.0%,APASL指南组51.1%,EASL指南组77.8%,EASL指南组90 d病死率显著高于CMA指南组(χ2=8.351,P=0.004)和APASL指南组(χ2=7.650,P=0.006);EASL指南对短期死亡风险预测的敏感度为22.2%,特异度为92.3%,对应的曲线下面积为0.576。 结论 符合EASL指南的慢加急性肝衰竭患者短期预后更差,该指南有助于识别短期死亡风险较高的患者。 Abstract:Objective To investigate the influence of different diagnostic criteria on the short-term prognosis of patients with acute-on-chronic liver failure (ACLF). Methods A total of 115 ACLF patients who were hospitalized in Department of Gastroenterology, The Second Affiliated Hospital of Kunming Medical University, from January 2018 to January 2022 were enrolled, and all patients received internal medical treatment combined with artificial liver therapy. According to the guidelines, the patients were divided into CMA guideline group (Diagnostic and treatment guidelines for liver failure by Chinese Medical Association)(n=100), APASL guideline group (Consensus statements of Asian Pacific Association for the Study of the Liver)(n=94), and EASL guideline group (Criteria proposed by European Association for the Study of the Liver)(n=36). The above three guidelines were compared in terms of 90-day mortality rate. A one-way analysis of variance was used for comprision of continuous date between groups; the chi-square test was used for comprision of categorical date between groups. The receiver operating characteristic (ROC) curve of related variables. Results The 90-day mortality rate was 50.0% in the CMA guideline group, 51.1% in the APASL guideline group, and 77.8% in the EASL guideline group, and the EASL guideline group had a significantly higher 90-day mortality rate than the CMA guideline group (χ2=8.351, P=0.004) and the APASL guideline group (χ2=7.650, P=0.006). EASL guideline had a sensitivity of 22.2% and a specificity of 92.3% in predicting the risk of short-term mortality, with an area under the ROC curve was 0.576. Conclusion ACLF patients who meet EASL guideline tend to have a worse short-term prognosis, and this guideline may help to identify patients at a relatively high risk of short-term death. -
Key words:
- Acute-On-Chronic Liver Failure /
- Liver, Artificial /
- Prognosis
-
表 1 一般资料比较
Table 1. Comparison of general data
项目 CMA指南组 (n=100) APASL指南组 (n=94) EASL指南组 (n=36) 统计值 P值 性别[例(%)] χ2=0.017 0.992 男 70(70.0) 65(69.1) 25(69.4) 女 30(30.0) 29(30.9) 11(30.6) 年龄(岁) 49.9±12.3 49.5±11.8 53.5±12.2 F=1.543 0.216 病因[例(%)] χ2=5.762 0.674 乙型肝炎 49(49.0) 46(48.9) 12(33.3) 丙型肝炎 2(2.0) 2(2.1) 1(2.8) 酒精性肝病 24(24.0) 23(24.5) 9(25.0) 自身免疫性肝病 11(11.0) 11(11.7) 4(11.1) 其他 14(14.0) 12(12.8) 10(27.8) 人工肝模式[例(%)] χ2=4.201 0.379 PE 27(27.0) 30(31.9) 16(44.4) DPMAS 55(55.0) 45(47.9) 15(41.7) PE+DPMAS 18(18.0) 19(20.2) 5(13.9) 人工肝次数(次) 3.3±1.7 3.3±1.6 2.7±1.2 F=2.137 0.120 住院时长(d) 19.4±8.2 19.6±8.0 16.2±7.0 F=2.663 0.072 90 d病死率[例(%)] 50(50.0)1) 48(51.1)1) 28(77.8) χ2=9.133 0.010 注:与EASL指南组比较,1) P<0.05。 表 2 3组赋值和人数统计
Table 2. Assignment and population statistics of the three groups
生存情况 赋值 1=CMA指南组 2=APASL指南组 3=EASL指南组 死亡(例) 50 48 28 存活(例) 50 46 8 合计(例) 100 94 36 -
[1] Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [2] LI H, CHEN LY, ZHANG NN, et al. Characteristics, diagnosis and prognosis of acute-on-chronic liver failure in cirrhosis associated to hepatitis B[J]. Sci Rep, 2016, 6: 25487. DOI: 10.1038/srep25487. [3] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [4] SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver(APASL): An update[J]. Hepatol Int, 2019, 13( 4): 353- 390. DOI: 10.1007/s12072-019-09946-3. [5] MOREAU R, JALAN R, GINES P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis[J]. Gastroenterology, 2013, 144( 7): 1426- 1437, 1437. DOI: 10.1053/j.gastro.2013.02.042. [6] ARROYO V, MOREAU R, JALAN R. Acute-on-chronic liver failure[J]. N Engl J Med, 2020, 382( 22): 2137- 2145. DOI: 10.1056/NEJMra1914900. [7] ZACCHERINI G, WEISS E, MOREAU R. Acute-on-chronic liver failure: Definitions, pathophysiology and principles of treatment[J]. JHEP Rep, 2020, 3( 1): 100176. DOI: 10.1016/j.jhepr.2020.100176. [8] LIU H, ZHANG Q, LIU L, et al. Effect of artificial liver support system on short-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure[J]. Artif Organs, 2020, 44( 10): E434- E447. DOI: 10.1111/aor.13710. [9] WU TZ, LI J, SHAO L, et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. Gut, 2018, 67( 12): 2181- 2191. DOI: 10.1136/gutjnl-2017-314641. [10] SARIN SK, KEDARISETTY CK, ABBAS Z, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver(APASL) 2014[J]. Hepatol Int, 2014, 8( 4): 453- 471. DOI: 10.1007/s12072-014-9580-2. [11] FAN Q, LI Z. Liver transplantation for acute-on-chronic liver failure[J]. Ogran Transplant, 2022, 13( 3): 333- 337. DOI: 10.3969/j.issn.1674-7445.2022.03.008.范祺, 李照. 慢加急性肝衰竭的肝移植治疗[J]. 器官移植, 2022, 13( 3): 333- 337. DOI: 10.3969/j.issn.1674-7445.2022.03.008. [12] Transplantation Immunology Committee of Branch of Organ Transplantation Physician of Chinese Medical Doctor Association, Enhanced Recovery of Liver Transplantation Group of Enhanced Recovery after Surgery Committee of Chinese Research Hospital Society. Expert consensus on perioperative management of liver transplantation in adults with acute-on-chronic liver failure[J]. Organ Transplantation, 2020, 11( 5): 533- 542. DOI: 10.3969/j.issn.1674-7445.2020.05.001.中国医师协会器官移植医师分会移植免疫学专业委员会, 中国研究型医院学会加速康复外科委员会肝移植加速康复学组. 成人慢加急性肝衰竭肝移植围手术期管理专家共识[J]. 器官移植, 2020, 11( 5): 533- 542. DOI: 10.3969/j.issn.1674-7445.2020.05.001. [13] ZHENG Z, LI X, LI ZL, et al. Artificial and bioartificial liver support systems for acute and acute-on-chronic hepatic failure: A meta-analysis and meta-regression[J]. Exp Ther Med, 2013, 6( 4): 929- 936. DOI: 10.3892/etm.2013.1241. [14] XIAO LL, XU XW, HUANG KZ, et al. Artificial liver support system improves short-term outcomes of patients with HBV-associated acute-on-chronic liver failure: A propensity score analysis[J]. Biomed Res Int, 2019, 2019: 3757149. DOI: 10.1155/2019/3757149. [15] ZHANG J, LUO H, HAN Y, et al. Sequential versus mono double plasma molecular adsorption system in acute-on-chronic liver failures: A propensity-score matched study[J]. Int J Artif Organs, 2022, 45( 1): 5- 13. DOI: 10.1177/0391398820987565. [16] European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis[J]. J Hepatol, 2018, 69( 2): 406- 460. DOI: 10.1016/j.jhep.2018.03.024. [17] ZHANG Q, LI Y, HAN T, et al. Comparison of current diagnostic criteria for acute-on-chronic liver failure[J]. PLoS One, 2015, 10( 3): e0122158. DOI: 10.1371/journal.pone.0122158. [18] WU J, LI YY, HU JH, et al. Differential characteristics and prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure defined by European Association for the Study of the Liver-Chronic Liver Failure criteria[J]. Hepatol Res, 2018, 48( 2): 153- 164. DOI: 10.1111/hepr.12909. [19] ZHU LC, ZENG JK, YUAN GC, et al. Survival advantage of patients with acute-on-chronic pre-liver failure treated with artificial liver: A multi-center study[J]. J Pract Med, 2022, 38( 19): 2434- 2439. DOI: 10.3969/j.issn.1006-5725.2022.19.011.朱龙川, 曾敬科, 袁桂才, 等. 慢加急性肝衰竭前期患者是人工肝治疗的生存优势人群: 一项多中心回顾性研究[J]. 实用医学杂志, 2022, 38( 19): 2434- 2439. DOI: 10.3969/j.issn.1006-5725.2022.19.011. [20] LEÃO GS, LUNARDI FL, PICON RV, et al. Acute-on-chronic liver failure: A comparison of three different diagnostic criteria[J]. Ann Hepatol, 2019, 18( 2): 373- 378. DOI: 10.1016/j.aohep.2019.01.001. [21] CAO ZJ, LIU YH, CAI MH, et al. The use of NACSELD and EASL-CLIF classification systems of ACLF in the prediction of prognosis in hospitalized patients with cirrhosis[J]. Am J Gastroenterol, 2020, 115( 12): 2026- 2035. DOI: 10.14309/ajg.0000000000000771. [22] MA YJ, DU LY, BAI L, et al. Assessment value of short-term prognosis of six predictive models for patients with acute-on-chronic liver failure treated with artificial liver support system[J]. J Sichuan Univ Med Sci, 2022, 53( 5): 758- 763. DOI: 10.12182/20220960203.马元吉, 杜凌遥, 白浪, 等. 六种预测模型对人工肝治疗的慢加急性肝衰竭患者短期预后的评估价值[J]. 四川大学学报(医学版), 2022, 53( 5): 758- 763. DOI: 10.12182/20220960203. -



 PDF下载 ( 656 KB)
PDF下载 ( 656 KB)

 下载:
下载:


