非HBV和非HCV感染相关肝细胞癌患者临床特征分析
DOI: 10.3969/j.issn.1001-5256.2023.10.013
-
摘要:
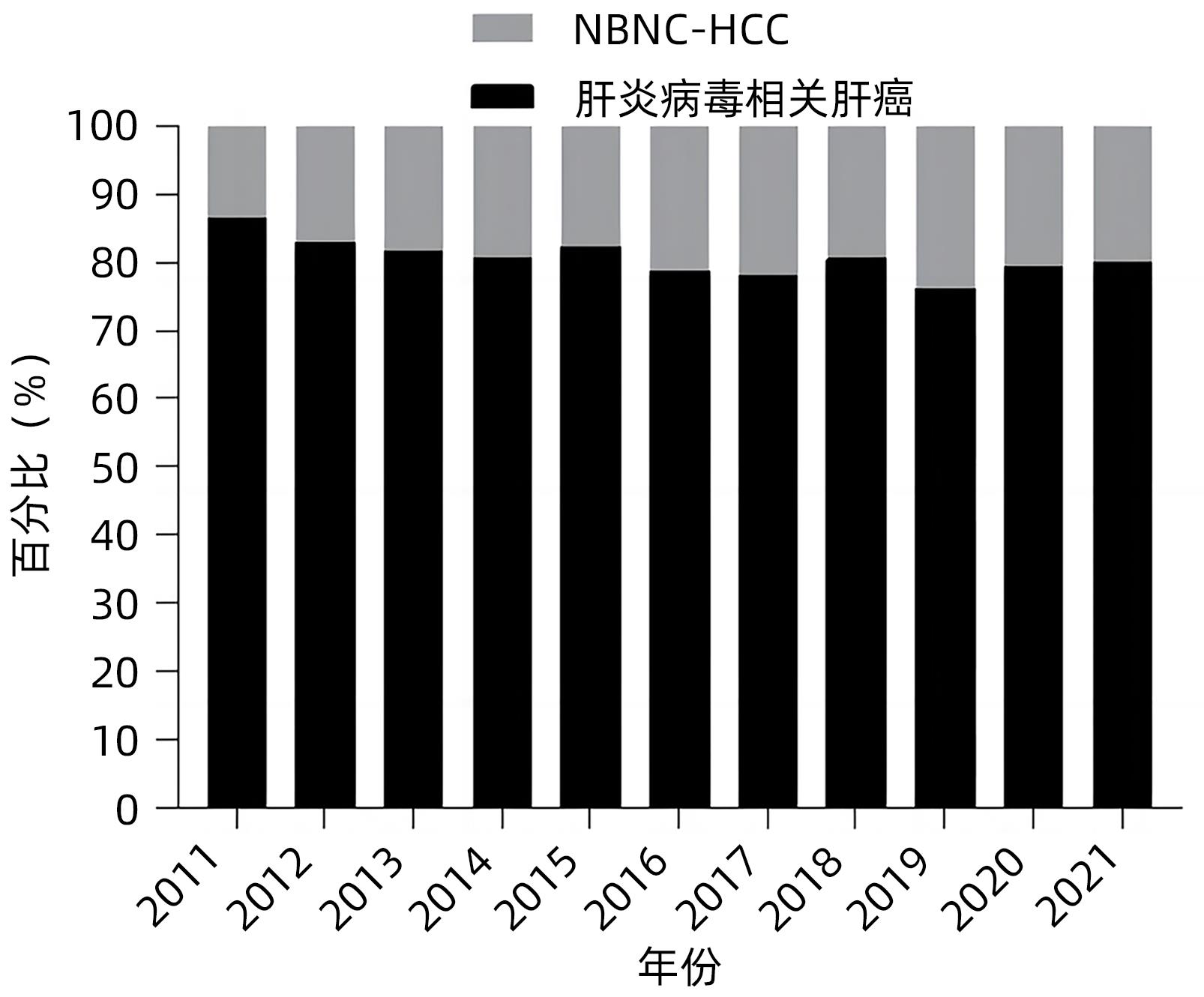
目的 了解非HBV和非HCV相关肝细胞癌(NBNC-HCC)在肝癌中占比变化情况,对NBNC-HCC的临床病理特征进行比较和分析。 方法 选取2011年1月—2021年12月在四川省人民医院诊断的HCC患者3 090例,根据肝炎标志物结果,分为肝炎病毒相关HCC组(n=2 472)和NBNC-HCC组(n=618),NBNC-HCC组患者根据背景肝病以及合并代谢危险因素情况,分为代谢异常HCC组(n=289)、酒精性肝病(ALD)相关HCC组(n=174)和其他HCC组(n=155)。收集所有HCC患者的一般资料、实验室指标、病理结果。计量资料两组间比较采用Mann-Whitney U检验,三组间比较采用Kruskal-Wallis H检验;计数资料组间比较采用χ2检验。NBNC-HCC在HCC中占比变化趋势采用趋势χ2检验。 结果 NBNC-HCC在肝癌患者中的占比从2011年13.7%增加到2021年20.1%(χ2=5.529,P=0.019),NBNC-HCC组与肝炎病毒相关HCC组患者相比,糖尿病和高血压占比较高(28.0% vs 10.3%,χ2=129.482,P<0.001;33.2% vs 15.2%,χ2=105.079,P<0.001),肝硬化和血管侵犯占比较低(44.5% vs 68.4%,χ2=122.563,P<0.001;20.4% vs 29.6%,χ2=7.749,P=0.005),BMI水平较高(Z=-4.015,P<0.001)。与ALD相关HCC组相比,代谢异常HCC组BMI指数较高、FIB-4指数较低、肝硬化比例较低(P值均<0.05)。 结论 NBNC-HCC患者在肝癌中占比呈上升趋势,NBNC-HCC合并肥胖、糖尿病和高血压等代谢危险因素较多。代谢异常HCC组患者可能在无肝硬化时或者肝纤维化早期发生肝癌。 -
关键词:
- 癌, 肝细胞 /
- 糖尿病 /
- 高血压 /
- 肝疾病, 酒精性 /
- 病理状态, 体征和症状
Abstract:Objective To investigate the change in the proportion of non-B, non-C hepatocellular carcinoma (NBNC-HCC) in hepatocellular carcinoma, and to compare and analyze the clinicopathological features of NBNC-HCC. Methods A total of 3 090 patients with hepatocellular carcinoma (HCC) who were diagnosed in Sichuan Provincial People’s Hospital from January 2011 to December 2021 were enrolled, and according to the hepatitis markers, they were divided into hepatitis virus infection-associated HCC group with 2 472 patients and NBNC-HCC group with 618 patients. According to the liver disease and metabolic risk factors, the NBNC-HCC group was further divided into metabolic disorder HCC group with 289 patients, alcoholic liver disease (ALD)-associated HCC group with 174 patients, and other HCC group with 155 patients. General information, laboratory markers, and pathological findings were collected from all HCC patients. The Mann-Whitney U test was used for comparison of continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between three groups; the chi-square test was used for comparison of categorical data between groups, and the chi-square trend test was used to investigate the trend of the change in the proportion of NBNC-HCC in HCC. Results The proportion of patients with NBNC-HCC in HCC increased from 13.7% in 2011 to 20.1% in 2021 (χ2=5.529, P=0.019), and compared with the hepatitis virus infection-associated HCC group, the NBNC-HCC group had a significantly higher proportion of patients with diabetes (28.0% vs 10.3%, χ2=129.482, P<0.001) or hypertension (33.2% vs 15.2%, χ2=105.079, P<0.001), a significantly lower proportion of patients with liver cirrhosis (44.5% vs 68.4%, χ2=122.563, P<0.001) or vascular invasion (20.4% vs 29.6%, χ2=7.749, P=0.005), and a significantly higher body mass index (BMI) (Z=-4.015, P<0.001). Compared with the ALD-HCC group, the metabolic disorder HCC group had a significantly higher BMI, a significantly lower FIB-4 index, and a significantly lower proportion of patients with liver cirrhosis (all P<0.05). Conclusion There is a tendency of increase in the proportion of patients with NBNC-HCC in HCC, and NBNC-HCC often coexists with metabolic risk factors such as obesity, diabetes, and hypertension. Patients in the metabolic disorder HCC group may develop liver cancer in the absence of liver cirrhosis or in the early stage of liver fibrosis. -
表 1 肝炎病毒相关HCC和NBNC-HCC临床特征比较
Table 1. Comparison of clinical features of hepatitis virus-associated HCC and NBNC-HCC
指标 肝炎病毒相关HCC(n=2 472) NBNC-HCC(n=618) 统计值 P值 年龄(岁) 55(46~63) 65(56~71) Z=-16.283 <0.001 男/女(例) 2 142/330 477/141 χ2=34.290 <0.001 BMI(kg/m2) 22.60(20.80~24.80) 23.38(21.12~25.51) Z=-4.015 <0.001 糖尿病[例(%)] 255(10.3) 173(28.0) χ2=129.482 <0.001 高血压[例(%)] 375(15.2) 205(33.2) χ2=105.079 <0.001 空腹血糖(mmol/L) 5.00(4.50~5.76) 5.47(4.77~6.80) Z=-8.917 <0.001 PLT(×109/L) 122(79~181) 149(101~211) Z=-7.246 <0.001 AST(U/L) 60(40~106) 46(31~78) Z=-8.185 <0.001 ALT(U/L) 48(31~76) 35(21~58) Z=-9.546 <0.001 TBil(μmoI/L) 20.2(14.4~29.3) 18.7(13.1~28.5) Z=-2.515 0.012 Alb(g/L) 36.4(32.3~40.2) 37.3(33.0~41.1) Z=-2.810 0.005 Cr(μmoI/L) 65.3(56.2~75.2) 66.3(56.0~76.2) Z=-0.982 0.326 ALBI分级(1/2/3,例) 614/1 629/229 200/360/58 χ2=15.123 0.001 AFP分级(1/2/3,例) 659/472/1 341 276/92/250 χ2=76.014 <0.001 肿瘤数量(单/多,例) 1 392/1 080 378/240 χ2=4.710 0.029 肿瘤直径(cm) 6.20(3.60~9.70) 6.15(3.80~9.20) Z=-0.254 0.800 肝硬化[例(%)] 1 692(68.4) 275(44.5) χ2=122.563 <0.001 FIB-4指数 4.18(2.40~7.73) 3.50(2.22~6.32) Z=-3.738 <0.001 Child分级(A/B/C,例) 1 624/669/179 424/158/36 χ2=2.471 0.291 CNLC分期(Ⅰ/Ⅱ/Ⅲ/Ⅳ,例) 889/416/969/198 254/74/238/52 χ2=11.035 0.012 表 2 肝炎病毒相关HCC和NBNC-HCC病理特征比较
Table 2. Comparison of pathological features of hepatitis virus-associated HCC and NBNC-HCC
病理特征 肝炎病毒相关HCC(n=918) NBNC-HCC(n=230) χ2值 P值 分化程度(低/中/高,例) 151/679/88 47/150/33 7.600 0.022 卫星病灶[例(%)] 199(21.7) 39(17.0) 2.494 0.114 脉管内癌栓[例(%)] 103(11.2) 30(13.0) 0.597 0.440 血管侵犯[例(%)] 272(29.6) 47(20.4) 7.749 0.005 表 3 肝炎病毒相关HCC患者在不同时间段的临床特征比较
Table 3. Comparison of clinical characteristics of patients with hepatitis virus-associated hepatocellular carcinoma at different periods
指标 2011年1月—2016年6月(n=898) 2016年7月—2021年12月(n=1 574) 统计值 P值 年龄(岁) 54(44~62) 55(47~64) Z=-4.296 <0.001 男/女(例) 788/110 1 354/220 χ2=1.475 0.224 BMI(kg/m2) 22.31(20.44~24.40) 22.84(20.82~24.97) Z=-3.529 <0.001 糖尿病[例(%)] 72(8.0) 183(11.6) χ2=8.048 0.005 高血压[例(%)] 102(11.4) 273(17.3) χ2=15.920 <0.001 空腹血糖(mmol/L) 4.87(4.37~5.50) 5.10(4.63~5.92) Z=-7.280 <0.001 PLT(×109/L) 125(79~179) 121(78~181) Z=-0.224 0.822 AST(U/L) 69(45~121) 56(37~98) Z=-6.771 <0.001 ALT(U/L) 50(34~81) 46(30~74) Z=-3.560 <0.001 TBil(μmoI/L) 20.1(14.0~30.6) 20.2(14.6~28.9) Z=-0.330 0.974 Alb(g/L) 36.6(32.0~40.3) 36.4(32.4~40.1) Z=-0.665 0.506 Cr(μmoI/L) 64.9(56.1~75.2) 65.5(56.3~75.1) Z=-0.583 0.560 ALBI分级(1/2/3,例) 239/562/97 375/1 067/132 χ2=7.745 0.021 AFP分级(1/2/3,例) 208/155/535 451/317/806 χ2=16.332 <0.001 肿瘤数量(单/多,例) 494/404 898/676 χ2=0.968 0.325 肿瘤直径(cm) 6.75(4.00~10.00) 5.90(3.40~9.60) Z=-4.039 <0.001 肝硬化[例(%)] 551(61.4) 1 141(72.5) χ2=32.807 <0.001 FIB-4指数 4.30(2.54~8.46) 4.12(2.32~7.38) Z=-2.108 0.035 Child分级(A/B/C,例) 564/257/77 1 060/412/102 χ2=6.518 0.038 CNLC分期(Ⅰ/Ⅱ/Ⅲ/Ⅳ,例) 339/177/299/83 550/239/670/115 χ2=23.427 <0.001 表 4 NBNC-HCC患者在不同时间段的临床特征比较
Table 4. Comparison of clinical characteristics of patients with non-B, non-C hepatocellular carcinoma at different periods
指标 2011年1月—2016年6月(n=188) 2016年7月—2021年12月(n=430) 统计值 P值 年龄(岁) 64(58~71) 65(54~72) Z=-0.529 0.597 男/女(例) 140/48 337/93 χ2=1.132 0.287 BMI(kg/m2) 22.62(20.57~25.21) 23.56(21.51~25.62) Z=-2.875 0.004 糖尿病[例(%)] 45(23.9) 128(29.8) χ2=2.207 0.137 高血压[例(%)] 55(29.3) 150(34.9) χ2=1.869 0.172 空腹血糖(mmol/L) 5.21(4.45~6.52) 5.58(4.90~6.93) Z=-3.342 0.001 PLT(×109/L) 148.50(102.75~214.00) 149.00(100.75~209.00) Z=-0.374 0.708 AST(U/L) 55(36~93) 43(30~72) Z=-3.693 <0.001 ALT(U/L) 36(23~54) 35(21~59) Z=-0.835 0.404 TBil(μmoI/L) 18.2(12.2~27.5) 19.0(13.2~28.6) Z=-0.800 0.424 Alb(g/L) 37.5(33.0~41.4) 37.2(32.9~40.9) Z=-0.292 0.770 Cr(μmoI/L) 65.0(55.0~75.7) 66.8(56.2~76.6) Z=-1.158 0.247 ALBI分级(1/2/3,例) 62/106/20 138/254/38 χ2=0.646 0.724 AFP分级(1/2/3,例) 81/25/82 195/67/168 χ2=1.277 0.528 肿瘤数量(单/多,例) 113/75 265/165 χ2=0.127 0.721 肿瘤直径(cm) 6.90(4.10~10.00) 5.85(3.60~9.09) Z=-2.475 0.013 肝硬化[例(%)] 63(33.5) 212(49.3) χ2=13.208 <0.001 FIB-4指数 4.05(2.36~6.85) 3.28(2.05~5.96) Z=-2.291 0.022 Child分级(A/B/C,例) 131/45/12 293/113/24 χ2=0.470 0.790 CNLC分期(Ⅰ/Ⅱ/Ⅲ/Ⅳ,例) 87/28/55/18 167/46/183/34 χ2=10.128 0.018 表 5 代谢异常HCC组、ALD相关HCC组和其他HCC组临床特征比较
Table 5. Comparison of clinical characteristics of metabolic abnormal liver cancer group, ALD-HCC group and other liver cancer groups
指标 代谢异常HCC组(n=289) ALD相关HCC组(n=174) 其他HCC组(n=155) 统计值 P值 年龄(岁) 66(56~73) 64(57~69) 63(54~71) H=6.909 0.032 男/女(例) 202/871) 170/42) 105/50 χ2=58.157 <0.001 BMI(kg/m2) 24.7(23.4~26.5)1)2) 23.1(20.8~25.3)2) 21.1(19.8~22.2) H=192.082 <0.001 糖尿病[例(%)] 128(44.3)1)2) 41(23.6)2) 4(2.6) χ2=89.434 <0.001 高血压[例(%)] 136(47.1)1)2) 51(29.3)2) 18(11.6) χ2=58.810 <0.001 空腹血糖(mmol/L) 5.9(5.1~7.2)2) 5.6(4.9~7.1)2) 4.8(4.4~5.5) H=77.649 <0.001 PLT(×109/L) 155.0(111.5~221.0)1) 128.0(83.8~181.8)2) 158.0(105.0~220.0) H=16.250 <0.001 AST(U/L) 41(30~67)1)2) 51(34~92) 55(33~86) H=13.773 0.001 ALT(U/L) 34.0(21.0~57.5) 38.0(23.0~60.3) 33.0(20.0~57.0) H=3.138 0.208 TBil(μmoI/L) 16.9(12.0~24.9)1) 21.3(16.1~37.4)2) 19.1(12.8~29.4) H=22.876 <0.001 Alb(g/L) 38.3(34.1~41.8)1)2) 35.9(31.4~40.5) 36.2(32.6~40.7) H=11.627 0.003 Cr(μmoI/L) 68.3(56.0~80.4)2) 66.3(57.7~75.4)2) 61.6(52.8~72.6) H=10.889 0.004 ALBI分级(1/2/3,例) 107/163/191) 45/106/23 48/91/16 χ2=9.996 0.04 AFP分级(1/2/3,例) 135/42/112 75/28/71 66/22/67 χ2=1.267 0.867 肿瘤数量(单/多,例) 190/99 97/77 91/64 χ2=5.095 0.078 肿瘤直径(cm) 6.1(3.8~9.2) 5.6(3.2~8.8)2) 6.5(4.3~10.0) H=7.040 0.030 肝硬化[例(%)] 110(38.1)1) 103(59.2)2) 62(40.0) χ2=19.527 <0.001 FIB-4指数 3.1(1.9~5.1)1) 4.4(2.6~9.0)2) 3.4(2.3~6.3) H=12.833 0.002 Child分级(A/B/C,例) 231/51/71)2) 93/59/222) 100/48/7 χ2=45.289 <0.001 CNLC分期(Ⅰ/Ⅱ/Ⅲ/Ⅳ,例) 134/32/111/121) 59/20/65/32) 61/22/62/10 χ2=28.334 <0.001 注:与ALD相关HCC组比较,1)P<0.05;与其他HCC组比较,2)P<0.05。 表 6 代谢异常HCC组、ALD-HCC组和其他HCC组病理特征比较
Table 6. Comparison of pathological characteristics of metabolically abnormal liver cancer group, ALD-HCC group and other liver cancer groups
病理特征 代谢异常HCC组(n=112) ALD相关HCC组(n=51) 其他HCC组 (n=67) χ2值 P值 分化程度(低/中/高,例) 27/71/14 6/35/10 14/44/9 4.061 0.398 卫星病灶[例(%)] 12(10.7)1) 8(15.7) 19(28.4) 9.343 0.009 脉管内癌栓[例(%)] 13(11.6) 6(11.8) 11(16.4) 0.950 0.622 血管侵犯[例(%)] 19(17.0) 11(21.6) 17(25.4) 1.875 0.392 注:与其他HCC组比较,1)P<0.05。 -
[1] LLOVET JM, KELLEY RK, VILLANUEVA A, et al. Hepatocellular carcinoma[J]. Nat Rev Dis Primers, 2021, 7( 1): 6. DOI: 10.1038/s41572-020-00240-3. [2] GOH GB, CHANG PE, TAN CK. Changing epidemiology of hepatocellular carcinoma in Asia[J]. Best Pract Res Clin Gastroenterol, 2015, 29( 6): 919- 928. DOI: 10.1016/j.bpg.2015.09.007. [3] XIAO L, ZHANG RL, ZHANG H, et al. Comparison of the clinical characteristics and survival between Uyghur patients with hepatitis virus-related and non-B, non-C hepatocellular carcinoma in Xinjiang, China[J]. Chin J Cancer Res, 2015, 27( 3): 279- 287. DOI: 10.3978/j.issn.1000-9604.2015.01.04. [4] NAGAOKI Y, HYOGO H, ANDO Y, et al. Increasing incidence of non-HBV- and non-HCV-related hepatocellular carcinoma: single-institution 20-year study[J]. BMC Gastroenterol, 2021, 21( 1): 306. DOI: 10.1186/s12876-021-01884-5. [5] MCGLYNN KA, PETRICK JL, EL-SERAG HB. Epidemiology of Hepatocellular Carcinoma[J]. Hepatology, 2021, 73 Suppl 1(Suppl 1): 4- 13. DOI: 10.1002/hep.31288. [6] TATEISHI R, UCHINO K, FUJIWARA N, et al. A nationwide survey on non-B, non-C hepatocellular carcinoma in Japan: 2011-2015 update[J]. J Gastroenterol, 2019, 54( 4): 367- 376. DOI: 10.1007/s00535-018-1532-5. [7] WAKIYAMA S, MATSUMOTO M, HARUKI K, et al. Clinical features and outcome of surgical patients with non-B non-C hepatocellular carcinoma[J]. Anticancer Res, 2017, 37( 6): 3207- 3213. DOI: 10.21873/anticanres.11682. [8] GOLABI P, RHEA L, HENRY L, et al. Hepatocellular carcinoma and non-alcoholic fatty liver disease[J]. Hepatol Int, 2019, 13( 6): 688- 694. DOI: 10.1007/s12072-019-09995-8. [9] LIN YP, WANG PM, CHUANG CH, et al. Metabolic risks are increasing in non-B non-C early-stage hepatocellular carcinoma: a 10-year follow-up study[J]. Front Oncol, 2022, 12: 816472. DOI: 10.3389/fonc.2022.816472. [10] KIM J, KANG W, SINN DH, et al. Potential etiology, prevalence of cirrhosis, and mode of detection among patients with non-B non-C hepatocellular carcinoma in Korea[J]. Korean J Intern Med, 2020, 35( 1): 65- 78. DOI: 10.3904/kjim.2018.040. [11] Chinese Diabetes Society. Guidelines for the prevention and treatment of type 2 diabetes in china(2020 edition)[J]. Int J Endocrinol Metab, 2021, 41( 5): 482- 548. DOI: 10.3760/cma.j.cn121383-20210825-08063.中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 国际内分泌代谢杂志, 2021, 41( 5): 482- 548. DOI: 10.3760/cma.j.cn121383-20210825-08063. [12] ESLAM M, NEWSOME PN, SARIN SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement[J]. J Hepatol, 2020, 73( 1): 202- 209. DOI: 10.1016/j.jhep.2020.03.039. [13] VITALE A, SVEGLIATI-BARONI G, ORTOLANI A, et al. Epidemiological trends and trajectories of MAFLD-associated hepatocellular carcinoma 2002-2033: the ITA.LI.CA database[J]. Gut, 2023, 72( 1): 141- 152. DOI: 10.1136/gutjnl-2021-324915. [14] Chinese Medical Association, Journal of Chinese Medical Association, Chinese Society of Gastroenterology, et al. Guideline for primary care of alcoholic liver disease(2019)[J]. Chin Gen Pract, 2020, 19( 11): 990- 996. DOI: 10.3760/cma.j.cn114798-20200812-00898.中华医学会, 中华医学会杂志社, 中华医学会消化病学分会, 等. 酒精性肝病基层诊疗指南(2019年)[J]. 中华全科医师杂志, 2020, 19( 11): 990- 996. DOI: 10.3760/cma.j.cn114798-20200812-00898. [15] Bureau of Medical Administration, National Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China(2019 edition)[J]. J Clin Hepatol, 2020, 36( 2): 277- 292. DOI: 10.3969/j.issn.1001-5256.2020.02.007.中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2020, 36( 2): 277- 292. DOI: 10.3969/j.issn.1001-5256.2020.02.007. [16] SHAH AG, LYDECKER A, MURRAY K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease[J]. Clin Gastroenterol Hepatol, 2009, 7( 10): 1104- 1112. DOI: 10.1016/j.cgh.2009.05.033. [17] JOHNSON PJ, BERHANE S, KAGEBAYASHI C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade[J]. J Clin Oncol, 2015, 33( 6): 550- 558. DOI: 10.1200/JCO.2014.57.9151. [18] ZHOU J, ZHOU F, WANG W, et al. Epidemiological features of NAFLD from 1999 to 2018 in China[J]. Hepatology, 2020, 71( 5): 1851- 1864. DOI: 10.1002/hep.31150. [19] LIU K, MCCAUGHAN GW. Epidemiology and etiologic associations of non-alcoholic fatty liver disease and associated HCC[J]. Adv Exp Med Biol, 2018, 1061: 3- 18. DOI: 10.1007/978-981-10-8684-7_2. [20] KANWAL F, KRAMER JR, LI L, et al. Effect of metabolic traits on the risk of cirrhosis and hepatocellular cancer in nonalcoholic fatty liver disease[J]. Hepatology, 2020, 71( 3): 808- 819. DOI: 10.1002/hep.31014. [21] DAVID D, RAGHAVENDRAN A, GOEL A, et al. Risk factors for non-alcoholic fatty liver disease are common in patients with non-B non-C hepatocellular carcinoma in India[J]. Indian J Gastroenterol, 2017, 36( 5): 373- 379. DOI: 10.1007/s12664-017-0785-x. [22] YAN SY, FAN JG. Diagnosis and treatment of hepatocellular carcinoma associated with non-alcoholic fatty liver disease[J]. J Clin Hepatol, 2021, 37( 8): 1748- 1752. DOI: 10.3969/j.issn.1001-5256.2021.08.002.颜士岩, 范建高. 非酒精性脂肪性肝病相关肝细胞癌的诊断和治疗[J]. 临床肝胆病杂志, 2021, 37( 8): 1748- 1752. DOI: 10.3969/j.issn.1001-5256.2021.08.002. [23] LEVRERO M, ZUCMAN-ROSSI J. Mechanisms of HBV-induced hepatocellular carcinoma[J]. J Hepatol, 2016, 64( 1 Suppl): S84-S101. DOI: 10.1016/j.jhep.2016.02.021. [24] YU MW, LIN CL, LIU CJ, et al. Influence of metabolic risk factors on risk of hepatocellular carcinoma and liver-related death in men with chronic hepatitis B: A large cohort study[J]. Gastroenterology, 2017, 153( 4): 1006- 1017.e 5. DOI: 10.1053/j.gastro.2017.07.001. [25] JIANG LN, LI W, ZHAO JM. Current status and perspectives of the clinical and basic research on concomitant chronic hepatitis B virus infection and nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2021, 37( 7): 1489- 1494. DOI: 10.3969/j.issn.1001-5256.2021.07.001.蒋丽娜, 李玮, 赵景民. 慢性HBV感染重叠非酒精性脂肪性肝病临床与基础研究的现状及展望[J]. 临床肝胆病杂志, 2021, 37( 7): 1489- 1494. DOI: 10.3969/j.issn.1001-5256.2021.07.001. [26] CHEN CL, YANG HI, YANG WS, et al. Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: a follow-up study in Taiwan[J]. Gastroenterology, 2008, 135( 1): 111- 121. DOI: 10.1053/j.gastro.2008.03.073. [27] STINE JG, WENTWORTH BJ, ZIMMET A, et al. Systematic review with meta-analysis: risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases[J]. Aliment Pharmacol Ther, 2018, 48( 7): 696- 703. DOI: 10.1111/apt.14937. [28] PERUMPAIL RB, LIU A, WONG RJ, et al. Pathogenesis of hepatocarcinogenesis in non-cirrhotic nonalcoholic fatty liver disease: Potential mechanistic pathways[J]. World J Hepatol, 2015, 7( 22): 2384- 2388. DOI: 10.4254/wjh.v7.i22.2384. [29] WHITE DL, KANWAL F, EL-SERAG HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review[J]. Clin Gastroenterol Hepatol, 2012, 10( 12): 1342- 1359.e 2. DOI: 10.1016/j.cgh.2012.10.001. [30] WONG DK, CHENG S, MAK LL, et al. Among patients with undetectable hepatitis B surface antigen and hepatocellular carcinoma, a high proportion has integration of HBV DNA into hepatocyte DNA and no cirrhosis[J]. Clin Gastroenterol Hepatol, 2020, 18( 2): 449- 456. DOI: 10.1016/j.cgh.2019.06.029. -



 PDF下载 ( 668 KB)
PDF下载 ( 668 KB)

 下载:
下载:


