74例特发性非硬化性门静脉高压症患者的临床特征分析
DOI: 10.3969/j.issn.1001-5256.2023.07.010
Clinical features of idiopathic non-cirrhotic portal hypertension: An analysis of 74 patients
-
摘要:
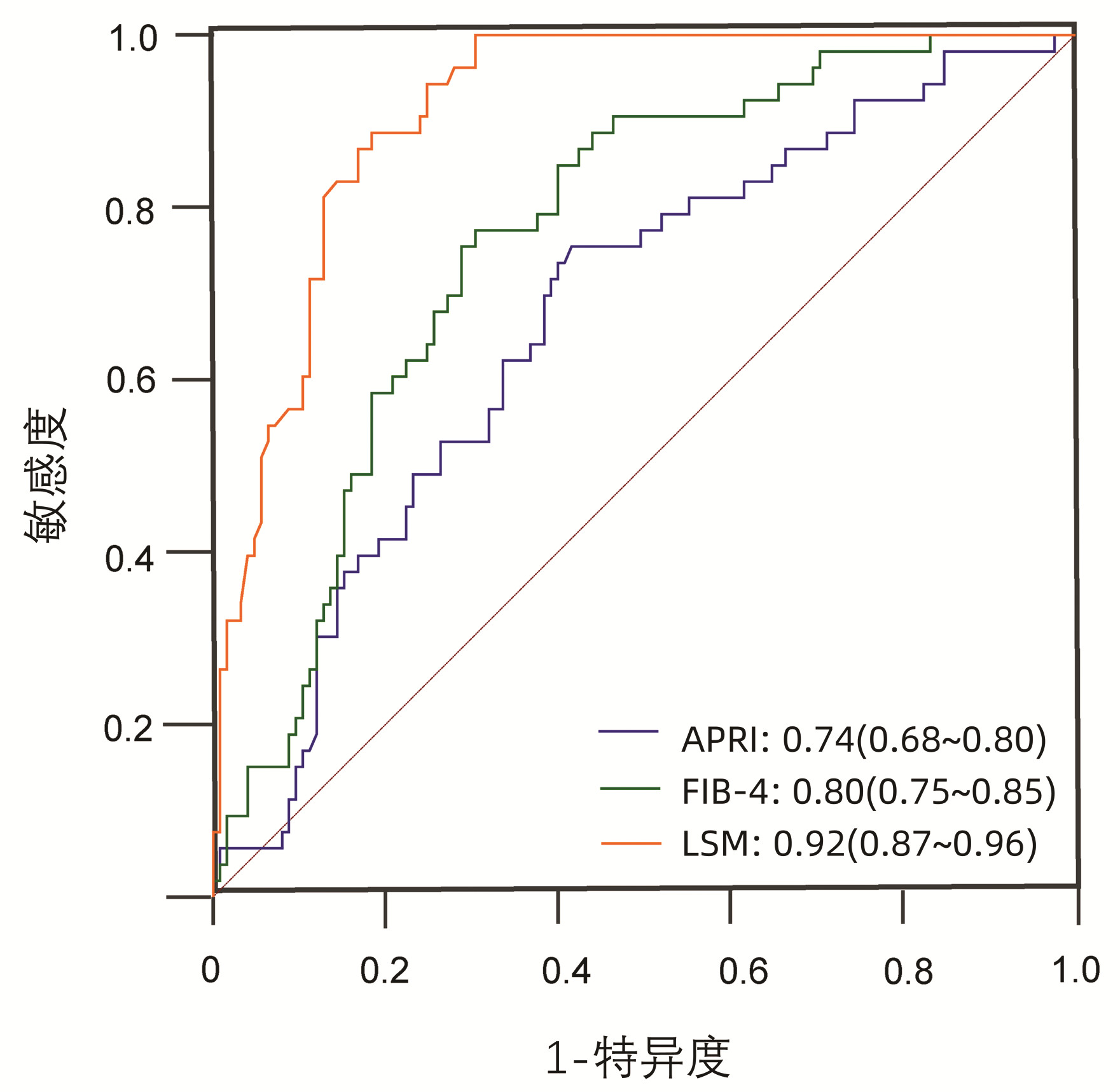
目的 特发性非硬化性门静脉高压(INCPH)是一种少见的引起门静脉高压的病因,对INCPH患者的临床特点进行分析以辅助诊断及鉴别诊断。 方法 选取北京佑安医院2019年1月—2022年7月经肝穿刺病理明确诊断为INCPH的住院患者74例,并以同期住院的332例肝硬化患者作为对照组,记录其人口学指标、实验室指标、胃镜、肝弹性检查、病理检查及并发症等资料,进行组间差异比较,并根据受试者工作特征曲线(ROC曲线)评价LSM、APRI、FIB-4对INCPH的鉴别诊断能力,采用DeLong检验方法进行ROC曲线下面积(AUC)比较。符合正态分布的计量资料两组间比较采用成组t检验,非正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ2检验。 结果 INCPH患者中46.55%的患者起病时无明显症状,43.24%患者曾被误诊为肝硬化。INCPH患者合并消化道出血比例明显多于肝硬化患者(62.16% vs 41.27%,χ2 =10.67,P<0.01),但合并中-重度腹水患者比例明显少于肝硬化患者(16.21% vs 29.82%,χ2=34.98,P<0.01),无肝性脑病发生。病理方面,89.19%(66/74)患者病理表现为典型的闭塞性门静脉病。INCPH患者肝功能指标、MELD评分、Child-Pugh评分等指标明显优于肝硬化患者,肝硬度值[9.05(7.18~12.33) vs 25.32(16.21~47.23),Z=-8.41,P<0.01]、APRI评分[0.70(0.41~1.28) vs 1.35 (0.80~2.39),Z=-6.21,P<0.01]、FIB-4指数[2.99(1.62~4.81) vs 6.68(4.06~10.42),Z=-8.39,P<0.01] 均较肝硬化低。LSM、FIB-4、APRI对INCPH与肝硬化患者具有很好的鉴别诊断能力,尤其是LSM的AUC达到0.92(0.87~0.96),敏感度和特异度分别为92.68%和81.60%。 结论 INCPH患者起病较隐匿,门静脉高压相关并发症发生率较高,而肝功能相对较好,尤其是LSM<14.5 kPa的患者,临床遇到此类患者需警惕INCPH可能。 -
关键词:
- 高血压, 门静脉 /
- 特发性非硬化性门静脉高压 /
- 肝硬化 /
- 并发症
Abstract:Objective Idiopathic non-cirrhotic portal hypertension (INCPH) is a rare cause of portal hypertension, and this study aims to analyze the clinical features of patients with INCPH, and to assist in diagnosis and differential diagnosis. Methods A total of 74 patients who were hospitalized in Beijing YouAn Hospital from January 2019 to July 2022 and were diagnosed with INCPH were enrolled, and 332 patients with liver cirrhosis who were hospitalized during the same period of time were enrolled as control group. Demographic data, laboratory markers, gastroscopy, liver elasticity, pathological examination, and complications were recorded and compared between the two groups. The receiver operating characteristic (ROC) curve was used to investigate the ability of liver stiffness measurement (LSM), aspartate aminotransferase-to-platelet ratio index (APRI), and fibrosis-4 (FIB-4) in the differential diagnosis of INCPH, and the DeLong test was used to compare the area under the ROC curve (AUC). The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test was used for comparison of categorical data between two groups. Results Among the patients with INCPH, 46.55% had no obvious symptoms at disease onset and 43.24% were misdiagnosed with liver cirrhosis. Compared with the patients with liver cirrhosis, the patients with INCPH had a significantly higher proportion of patients with gastrointestinal bleeding (62.16% vs 41.27%, χ2=10.67, P < 0.01) and a significantly lower proportion of patients with moderate-to-severe ascites (16.21% vs 29.82%, χ2=34.98, P < 0.01), and there were few patients with hepatic encephalopathy. As for pathology, 89.19% (66/74) of the INCPH patients manifested as typical occlusive portal vein disease. The statistical analysis showed that compared with the patients with liver cirrhosis, the patients with INCPH had significantly better liver function parameters, MELD score, and Child-Pugh score and significantly lower LSM [9.05(7.18-12.33) vs 25.32(16.21-47.23), Z=-8.41, P < 0.01], APRI score [0.70(0.41-1.28) vs 1.35(0.80-2.39), Z=-6.21, P < 0.01], and FIB-4 index [2.99(1.62-4.81) vs 6.68(4.06-10.42), Z=-8.39, P < 0.01]. LSM, FIB-4, and APRI had a good ability in differentiating INCPH from liver cirrhosis, and in particular, LSM had an AUC of up to 0.92 (95% confidence interval: 0.87-0.96), with a sensitivity of 92.68% and a specificity of 81.60%. Conclusion INCPH patients tend to have an insidious onset, a relatively high incidence rate of portal hypertension-related complications, and relatively good liver function, especially the patients with LSM < 14.5 kPa. The possibility of INCPH should be considered for such patients in clinical practice. -
表 1 INCPH与肝硬化患者临床特征比较
Table 1. Comparison of clinical characteristics between INCPH and liver cirrhosis
指标 肝硬化(n=332) INCPH(n=74) 统计值 P值 性别[例(%)] χ2=10.67 <0.01 男 228 (68.67) 36(48.65) 女 104(31.33) 38(51.35) 年龄(岁) 55.94±11.64 47.53±16.18 t=4.75 <0.01 WBC(×109/L) 3.60(2.48~5.38) 2.99(2.30~4.84) Z=-1.56 0.12 NEUT% 60.98±12.90 62.86±12.92 t=-1.25 0.21 Hb(g/L) 98.84±28.06 106.61±28.42 t=-2.38 0.02 PLT(×109/L) 71.00(50.00~105.50) 88.50(62.00~143.25) Z=-2.90 <0.01 ALT(U/L) 21.02(13.20~31.41) 19.50(13.75~28.53) Z=-0.29 0.77 AST(U/L) 35.22(25.25~57.14) 25.35(20.26~31.25) Z=-6.15 <0.01 TBil(μmol/L) 35.40(21.13~87.83) 17.80(12.95~26.42) Z=-7.89 <0.01 Alb(g/L) 31.92±5.61 37.69±5.16 t=-8.96 <0.01 Cr(mmol/L) 61(51~76) 56(47~71) Z=-2.22 0.03 eGFR(mL·min-1·1.73 m-2) 101.91(87.35~111.55) 109.85(97.53~121.33) Z=-3.75 <0.01 PT(s) 15.40(13.60~18.78) 13.10(12.30~13.80) Z=-8.59 <0.01 PTA(%) 61.55±19.50 79.85±12.05 t=-11.16 <0.01 INR 1.38(1.21~1.67) 1.17(1.10~1.23) Z=-8.09 <0.01 D-Dimer(μg/L) 493.5(201.5~1112.0) 200.2(98.3~450.5) Z=-5.38 <0.01 FIB(g/L) 1.63(1.24~2.15) 2.25(1.91~2.69) Z=-7.41 <0.01 CAP(dB/m) 232.3±51.5 223.5±22.4 t=0.953 0.34 LSM(kPa) 25.32(16.21~47.23) 9.05(7.18~12.33) Z=-8.41 <0.01 表 2 INCPH与肝硬化患者临床评分比较
Table 2. Comparison between clinical scores between INCPH and liver cirrhosis
临床评分 肝硬化(n=332) INCPH(n=74) 统计值 P值 APRI评分 1.35(0.80~2.39) 0.70(0.41~1.28) Z=-6.21 <0.01 FIB-4指数 6.68(4.06~10.42) 2.99(1.62~4.81) Z=-8.39 <0.01 MELD评分 8.13(4.18~12.19) 5.35(1.96~7.83) Z=-4.67 <0.01 Child-Pugh评分 8(7~11) 6(5~6) Z=-9.84 <0.01 Child-Pugh分级[例(%)] χ2=86.41 <0.01 A级 80(24.10) 59(79.73) B级 135(40.66) 14(18.92) C级 117(35.24) 1(1.35) 表 3 INCPH与肝硬化患者肝硬化相关并发症比较
Table 3. Comparison of cirrhotic-related complications between INCPH and liver cirrhosis
并发症 肝硬化(n=332) INCPH(n=74) χ2值 P值 上消化道出血[例(%)] 10.67 <0.01 否 195(58.73) 28(37.84) 是 137(41.27) 46(62.16) 腹水[例(%)] 34.98 <0.01 无 110(33.13) 47(63.51) 轻度 123(37.05) 15(20.27) 中度 80(24.10) 3(4.05) 重度 19(5.72) 9(12.16) 肝性脑病[例(%)] 15.69 <0.01 否 272(81.93) 74(100.00) 是 60(18.07) 0(0.00) 食管静脉曲张[例(%)] 15.28 <0.01 无 63(25.82) 3(5.36) 轻度 57(23.36) 13(23.21) 中度 58(23.77) 13(23.21) 重度 66(27.05) 27(48.21) 红色征[例(%)] 8.59 <0.01 阴性 140(57.38) 20(35.71) 阳性 104(42.62) 36(64.29) 表 4 LSM、FIB-4、APRI对INCPH鉴别诊断的ROC曲线结果
Table 4. ROC results of LSM, FIB-4 and APRI to perform differential diagnosis of INCPH
指标 AUC(95%CI) 截断值 敏感度(%) 特异度(%) 准确性 阳性似然比 阴性似然比 阳性预测值 阴性预测值 LSM 0.92(0.87~0.96) 14.50 92.68 81.60 0.84 5.04 0.09 0.62 0.97 FIB-4 0.80(0.75~0.85) 5.65 87.50 60.73 0.66 2.23 0.21 0.32 0.96 APRI 0.74(0.68~0.80) 0.92 69.86 67.98 0.68 2.18 0.44 0.33 0.91 LSM+FIB-4 0.92(0.88~0.96) -1.93 76.00 100.00 0.82 4.17 0.00 0.58 1.00 LSM+APRI 0.91(0.87~0.96) -1.07 80.80 92.68 0.84 4.83 0.09 0.61 0.97 -
[1] Chinese Society of Spleen and Portal Hypertension Surgery, Chinese Society of Surgery, Chinese Medical Association. Chinese expert consensus on clinical diagnosis and treatment of portal hypertension with hepatocellular carcinoma (2022 edition)[J]. Chin J Dig Surg, 2022, 21(4): 444-455. DOI: 10.3760/cma.j.cn115610-20220223-00104.中华医学会外科学分会脾及门静脉高压外科学组. 门静脉高压合并肝细胞癌临床诊断与治疗中国专家共识(2022版)[J]. 中华消化外科杂志, 2022, 21(4): 444-455. DOI: 10.3760/cma.j.cn115610-20220223-00104. [2] HUANG D, CAO JG, YE HY, et al. Occurrence and progression of hemodynamic dysfunction in cirrhotic portal hypertension[J]. Chin J Dig Surg, 2021, 20(10): 1117-1122. DOI: 10.3760/cma.j.cn115610-20210813-00394.黄登, 曹君贵, 叶航羊, 等. 肝硬化门静脉高压血流动力学紊乱发生及发展机制[J]. 中华消化外科杂志, 2021, 20(10): 1117-1122. DOI: 10.3760/cma.j.cn115610-20210813-00394. [3] XU JH, YU YY, XU XY. Current status of the clinical management of non-cirrhotic portal hypertension[J]. J Clin Hepatol, 2022, 38(7): 1457-1459. DOI: 10.3969/j.issn.1001-5256.2022.07.001.徐京杭, 于岩岩, 徐小元. 非肝硬化性门静脉高压症的临床管理现状[J]. 临床肝胆病杂志, 2022, 38(7): 1457-1459. DOI: 10.3969/j.issn.1001-5256.2022.07.001. [4] European Association for the Study of the Liver. EASL clinical practice guidelines: vascular diseases of the liver[J]. J Hepatol, 2016, 64(1): 179-202. DOI: 10.1016/j.jhep.2015.07.040. [5] KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33(2): 464-470. DOI: 10.1053/jhep.2001.22172. [6] WAI CT, GREENSON JK, FONTANA RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C[J]. Hepatology, 2003, 38(2): 518-526. DOI: 10.1053/jhep.2003.50346. [7] TESHALE E, LU M, RUPP LB, et al. APRI and FIB-4 are good predictors of the stage of liver fibrosis in chronic hepatitis B: the Chronic Hepatitis Cohort Study (CHeCS)[J]. J Viral Hepat, 2014, 21(12): 917-920. DOI: 10.1111/jvh.12279. [8] SATO Y, REN XS, HARADA K, et al. Induction of elastin expression in vascular endothelial cells relates to hepatoportal sclerosis in idiopathic portal hypertension: possible link to serum anti-endothelial cell antibodies[J]. Clin Exp Immunol, 2012, 167(3): 532-542. DOI: 10.1111/j.1365-2249.2011.04530.x. [9] SCHOUTEN JN, GARCIA-PAGAN JC, VALLA DC, et al. Idiopathic noncirrhotic portal hypertension[J]. Hepatology, 2011, 54(3): 1071-1081. DOI: 10.1002/hep.24422. [10] GOEL A, ELIAS JE, EAPEN CE, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension (NCIPH)-newer insights into pathogenesis and emerging newer treatment options[J]. J Clin Exp Hepatol, 2014, 4(3): 247-256. DOI: 10.1016/j.jceh.2014.07.005. [11] de GOTTARDI A, RAUTOU PE, SCHOUTEN J, et al. Porto-sinusoidal vascular disease: proposal and description of a novel entity[J]. Lancet Gastroenterol Hepatol, 2019, 4(5): 399-411. DOI: 10.1016/S2468-1253(19)30047-0. [12] OKUDAIRA M, OHBU M, OKUDA K. Idiopathic portal hypertension and its pathology[J]. Semin Liver Dis, 2002, 22(1): 59-72. DOI: 10.1055/s-2002-23207. [13] PULVIRENTI F, PENTASSUGLIO I, MILITO C, et al. Idiopathic non cirrhotic portal hypertension and spleno-portal axis abnormalities in patients with severe primary antibody deficiencies[J]. J Immunol Res, 2014, 2014: 672458. DOI: 10.1155/2014/672458. [14] GUIDO M, SARCOGNATO S, SACCHI D, et al. Pathology of idiopathic non-cirrhotic portal hypertension[J]. Virchows Arch, 2018, 473(1): 23-31. DOI: 10.1007/s00428-018-2355-8. [15] EAPEN CE, NIGHTINGALE P, HUBSCHER SG, et al. Non-cirrhotic intrahepatic portal hypertension: associated gut diseases and prognostic factors[J]. Dig Dis Sci, 2011, 56(1): 227-235. DOI: 10.1007/s10620-010-1278-2. [16] CAZALS-HATEM D, HILLAIRE S, RUDLER M, et al. Obliterative portal venopathy: portal hypertension is not always present at diagnosis[J]. J Hepatol, 2011, 54(3): 455-461. DOI: 10.1016/j.jhep.2010.07.038. [17] VERNIER-MASSOUILLE G, COSNES J, LEMANN M, et al. Nodular regenerative hyperplasia in patients with inflammatory bowel disease treated with azathioprine[J]. Gut, 2007, 56(10): 1404-1409. DOI: 10.1136/gut.2006.114363. [18] SANTRA A, DAS GUPTA J, DE BK, et al. Hepatic manifestations in chronic arsenic toxicity[J]. Indian J Gastroenterol, 1999, 18(4): 152-155. [19] GUIDO M, ALVES V, BALABAUD C, et al. Histology of portal vascular changes associated with idiopathic non-cirrhotic portal hypertension: nomenclature and definition[J]. Histopathology, 2019, 74(2): 219-226. DOI: 10.1111/his.13738. [20] MADHU K, AVINASH B, RAMAKRISHNA B, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension: common cause of cryptogenic intrahepatic portal hypertension in a Southern Indian tertiary hospital[J]. Indian J Gastroenterol, 2009, 28(3): 83-87. DOI: 10.1007/s12664-009-0030-3. [21] NAYAK NC, JAIN D, SAIGAL S, et al. Non-cirrhotic portal fibrosis: one disease with many names? An analysis from morphological study of native explant livers with end stage chronic liver disease[J]. J Clin Pathol, 2011, 64(7): 592-598. DOI: 10.1136/jcp.2010.087395. [22] de FRANCHIS R, BOSCH J, GARCIA-TSAO G, et al. Baveno VⅡ - Renewing consensus in portal hypertension[J]. J Hepatol, 2022, 76(4): 959-974. DOI: 10.1016/j.jhep.2021.12.022. [23] SEIJO S, REVERTER E, MIQUEL R, et al. Role of hepatic vein catheterisation and transient elastography in the diagnosis of idiopathic portal hypertension[J]. Dig Liver Dis, 2012, 44(10): 855-860. DOI: 10.1016/j.dld.2012.05.005. [24] KHANNA R, SARIN SK. Non-cirrhotic portal hypertension - diagnosis and management[J]. J Hepatol, 2014, 60(2): 421-441. DOI: 10.1016/j.jhep.2013.08.013. -



 PDF下载 ( 2041 KB)
PDF下载 ( 2041 KB)

 下载:
下载:


