胆道菌群导致原发性肝内胆管结石形成机理的研究进展
DOI: 10.3969/j.issn.1001-5256.2022.02.045
Research advances in the formation mechanism of primary intrahepatic stones caused by biliary flora
-
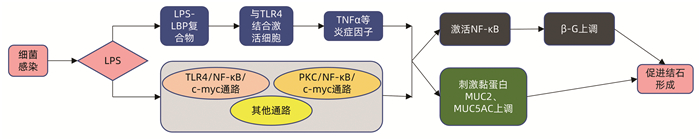
摘要: 原发性肝内胆管结石(PIS)是我国西南地区高发和难治性疾病,在初始治疗后,部分患者仍需要再次甚至多次手术。近年来有大量研究发现部分特异性菌群能在肝内胆管定植,导致胆道系统慢性感染及炎症。这些特异菌群可产生β-葡萄糖醛酸苷酶等代谢产物,在色素性结石的形成中起着重要作用,被称为“致石菌群”。本文对PIS发病机理中致石菌群的作用研究进展予以分析探讨,以期为PIS患者提供更多的治疗方式。Abstract: Primary intrahepatic stones (PIS) is a refractory disease with a high incidence rate in southwest China, and some patients still require surgery again or even more times after initial treatment. Many studies in recent years have shown that some specific flora can colonize in the intrahepatic bile duct, leading to chronic infection and inflammation of the biliary system, and these specific types of flora, called "stone-causing flora", can produce metabolites such as β-glucuronidase and play an important role in the formation of pigmented stones. This article analyzes the role of stone-causing flora in the pathogenesis of PIS, so as to provide more treatment options for PIS patients.
-
Key words:
- Primary Intrahepatic Stones /
- Biliary Flora /
- Pathologic Processes
-
表 1 肝内胆管结石菌群的相关研究结果
研究者 年份 样本 菌群结果 Tabata等[14] 1984 胆汁 检出率依次为:大肠杆菌、克雷伯氏菌、链球菌、绿脓杆菌 傅华群等[17] 1989 结石 厌氧菌占74.0%,需氧菌占98.0% Sheen-chen等[18] 2000 胆汁 检出率依次为:克雷伯氏菌、大肠杆菌、假单胞菌和肠球菌 Chang等[19] 2002 胆汁 革兰阴性菌为主,主要为大肠杆菌、克雷伯氏菌 Wu等[20] 2006 胆汁和结石 检出率依次为:肠球菌、大肠杆菌及克雷伯氏菌 李绍强等[21] 2009 胆汁 61.7%为革兰阴性菌,38.3%为革兰阳性菌 贾淑芹等[22] 2012 胆汁 检出率依次为大肠杆菌、肠球菌、克雷伯氏菌、假单孢菌和肠杆菌 陈安妮等[23] 2017 胆汁 检出率依次为:大肠杆菌、克雷伯氏菌及铜绿假单胞菌 吴樟强[24] 2017 胆汁 检出率依次为:大肠杆菌、粪肠球菌、克雷伯氏菌 包文中[25] 2006 胆管黏膜和胆汁 检出幽门螺杆菌和幽门螺杆菌感染相关蛋白 表 2 肝内胆管结石胆汁或结石细菌谱
需氧菌 胆汁或结石阳性率(%) 厌氧菌 胆汁或结石阳性率(%) 大肠杆菌 30.5~36.0 梭状芽孢杆菌 3.0~12.7 克雷伯氏菌 8.5~15.0 拟杆菌 0.5~8.0 肠球菌 5.0~9.1 链球菌属 3.0~10.0 粪肠球菌 2.6~29.8 -
[1] Biliary Tract Group, Chinese Society of Surgery, Chinese Medical Association. Guidelines for the diagnosis and treatment of hepatolithiasis[J]. Chin J Dig Surg, 2007, 6(2): 156-161. DOI: 10.3760/cma.j.issn.1673-9752.2007.02.028.中华医学会外科学分会胆道外科学组. 肝胆管结石病诊断治疗指南[J]. 中华消化外科杂志, 2007, 6(2): 156-161. DOI: 10.3760/cma.j.issn.1673-9752.2007.02.028. [2] CLEMENTE G, de ROSE AM, MURRI R, et al. Liver resection for primary intrahepatic stones: Focus on postoperative infectious complications[J]. World J Surg, 2016, 40(2): 433-439. DOI: 10.1007/s00268-015-3227-x. [3] SUZUKI Y, MORI T, YOKOYAMA M, et al. Hepatolithiasis: Analysis of Japanese nationwide surveys over a period of 40 years[J]. J Hepatobiliary Pancreat Sci, 2014, 21(9): 617-622. DOI: 10.1002/jhbp.116. [4] PENG JX, WANG LZ, DIAO JF, et al. Major hepatectomy for primary hepatolithiasis: A comparative study of laparoscopic versus open treatment[J]. Surg Endosc, 2018, 32(10): 4271-4276. DOI: 10.1007/s00464-018-6176-2. [5] PARK JS, JEONG S, LEE DH, et al. Risk factors for long-term outcomes after initial treatment in hepatolithiasis[J]. J Korean Med Sci, 2013, 28(11): 1627-1631. DOI: 10.3346/jkms.2013.28.11.1627. [6] YANG Y, RUAN Y, RUAN XM. Analysis on incidence and risk factors of postoperative nosocomial infection in patients with hepatolithiasis[J]. Med & Pharm J Chin PLA, 2021, 33(1): 58-61. DOI: 10.3969/j.issn.2095-140X.2021.01.013.杨滢, 阮勇, 阮小毛. 肝内胆管结石患者术后院内感染发生情况及危险因素分析[J]. 解放军医药杂志, 2021, 33(1): 58-61. DOI: 10.3969/j.issn.2095-140X.2021.01.013. [7] GUO P, BIE P. Interpretation of expert consensus on application of choledochoscope in diagnosis and treatment of hepatolithiasis (2019 edition)[J]. J Clin Hepatol, 2020, 36(1): 57-58. DOI: 10.3969/j.issn.1001-5256.2020.01.012.郭鹏, 别平. 《胆道镜在肝胆管结石病诊断与治疗中的应用专家共识(2019版)》解读[J]. 临床肝胆病杂志, 2020, 36(1): 57-58. DOI: 10.3969/j.issn.1001-5256.2020.01.012. [8] SHANG D, ZHANG GX, ZHANG QK. Minimally invasive integrated traditional Chinese and Western medicine therapy for hepatolithiasis based on the SELECT concept[J]. J Clin Hepatol, 2020, 36(1): 31-35. DOI: 10.3969/j.issn.1001-5256.2020.01.005.尚东, 张桂信, 张庆凯. 基于SELECT理念的中西医结合微创治疗肝胆管结石[J]. 临床肝胆病杂志, 2020, 36(1): 31-35. DOI: 10.3969/j.issn.1001-5256.2020.01.005. [9] TSUI WM, LAM PW, LEE WK, et al. Primary hepatolithiasis, recurrent pyogenic cholangitis, and oriental cholangiohepatitis: A tale of 3 countries[J]. Adv Anat Pathol, 2011, 18(4): 318-328. DOI: 10.1097/PAP.0b013e318220fb75. [10] MAKI T. Pathogenesis of calcium bilirubinate gallstone: Role of E. coli, beta-glucuronidase and coagulation by inorganic ions, polyelectrolytes and agitation[J]. Ann Surg, 1966, 164(1): 90-100. DOI: 10.1097/00000658-196607000-00010. [11] TAJEDDIN E, SHERAFAT SJ, MAJIDI MR, et al. Association of diverse bacterial communities in human bile samples with biliary tract disorders: A survey using culture and polymerase chain reaction-denaturing gradient gel electrophoresis methods[J]. Eur J Clin Microbiol Infect Dis, 2016, 35(8): 1331-1339. DOI: 10.1007/s10096-016-2669-x. [12] JIMÉNEZ E, SÁNCHEZ B, FARINA A, et al. Characterization of the bile and gall bladder microbiota of healthy pigs[J]. Microbiologyopen, 2014, 3(6): 937-949. DOI: 10.1002/mbo3.218. [13] MOLINERO N, RUIZ L, MILANI C, et al. The human gallbladder microbiome is related to the physiological state and the biliary metabolic profile[J]. Microbiome, 2019, 7(1): 100. DOI: 10.1186/s40168-019-0712-8. [14] TABATA M, NAKAYAMA F. Bacteriology of hepatolithiasis[J]. Prog Clin Biol Res, 1984, 152: 163-174. [15] TURNBAUGH PJ, GORDON JI. An invitation to the marriage of metagenomics and metabolomics[J]. Cell, 2008, 134(5): 708-713. DOI: 10.1016/j.cell.2008.08.025. [16] LU JY, WANG J. Advances in the pathogenesis of primary intrahepatic cholelithiasis[J]. Chin J Hepatobiliary Surg, 2011, 17(2): 168-170. DOI: 10.3760/cma.j.issn.1007-8118.2011.02.030.鲁嘉越, 王坚. 原发性肝内胆管结石成因研究现状[J]. 中华肝胆外科杂志, 2011, 17(2): 168-170. DOI: 10.3760/cma.j.issn.1007-8118.2011.02.030. [17] FU HQ, LI JY, HUANG SY. Anaerobes in biliary tract infection[J]. Chin J Surg, 1989, 27(8): 454-456, 507. DOI: 10.3760/j:issn:0529-5815.1989.08.003傅华群, 李建业, 黄淑云. 胆道厌氧菌感染的研究[J]. 中华外科杂志, 1989, 27(8): 454-456, 507. DOI: 10.3760/j:issn:0529-5815.1989.08.003 [18] SHEEN-CHEN S, CHEN W, ENG H, et al. Bacteriology and antimicrobial choice in hepatolithiasis[J]. Am J Infect Control, 2000, 28(4): 298-301. DOI: 10.1067/mic.2000.107071. [19] CHANG WT, LEE KT, WANG SR, et al. Bacteriology and antimicrobial susceptibility in biliary tract disease: An audit of 10-year's experience[J]. Kaohsiung J Med Sci, 2002, 18(5): 221-228. [20] WU SD, YU H, SUN JM. Bacteriological and electron microscopic examination of primary intrahepatic stones[J]. Hepatobiliary Pancreat Dis Int, 2006, 5(2): 228-231. [21] LI SQ, LIANG LJ, HUA YP, et al. Bacterial spectrum of bile in patients with intrahepatic stone and its clinical significance[J/CD]. Chin Arch Gen Surg (Electronic Edition), 2009, 3(4): 313-316. DOI: 10.3969/j.issn.1674-0793.2009.04.014.李绍强, 梁力建, 华赟鹏, 等. 肝内胆管结石患者胆汁的细菌谱及临床意义[J/CD]. 中华普通外科学文献(电子版), 2009, 3(4): 313-316. DOI: 10.3969/j.issn.1674-0793.2009.04.014. [22] JIA SQ, FU Q, JIN S. Bacterial spectrum of hepatolithiasis with biliary tract infection[J]. World Chin J Dig, 2012, 20(34): 3349-3353. https://www.cnki.com.cn/Article/CJFDTOTAL-XXHB201234022.htm贾淑芹, 福泉, 金山. 肝内胆管结石合并胆道感染的细菌谱[J]. 世界华人消化杂志, 2012, 20(34): 3349-3353. https://www.cnki.com.cn/Article/CJFDTOTAL-XXHB201234022.htm [23] CHEN AN, WANG H, ZHOU YN, et al. Supervision of the main pathogenic bacteria resistance rates and rationality analysis of antibacterial drugs usage in hepatolithiasis with biliary tract infection[J]. Acad J Guangdong Pharm Coll, 2017, 33(3): 388-392. DOI: 10.16809/j.cnki.2096-3653.2017011204.陈安妮, 王慧, 周燕妮, 等. 肝内胆管结石病原菌监测及抗菌药物使用合理性分析[J]. 广东药学院学报, 2017, 33(3): 388-392. DOI: 10.16809/j.cnki.2096-3653.2017011204. [24] WU ZQ. The relationship between bile bacterial spectrum and postoperative infection in patients with intrahepatic bile duct stones[D]. Fuzhou: Fujian Medical University, 2017.吴樟强. 肝内胆管结石患者胆汁细菌谱与术后感染的关系[D]. 福州: 福建医科大学, 2017. [25] BAO WZ. The relationship between Helicobacter pylori and primary intrahepatic bile duct stones[D]. Hefei: Anhui Medical University, 2006.包文中. 幽门螺杆菌与原发性肝内胆管结石之间的关系[D]. 合肥: 安徽医科大学, 2006. [26] BELZER C, KUSTERS JG, KUIPERS EJ, et al. Urease induced calcium precipitation by Helicobacter species may initiate gallstone formation[J]. Gut, 2006, 55(11): 1678-1679. DOI: 10.1136/gut.2006.098319. [27] WU T. The relationship between the diversity of intestinal flora and biliary tract flora and gallstone disease[D]. Kunming: Kunming Medical University, 2014.吴韬. 肠道菌群和胆道菌群多样性与胆石病的相关性研究[D]. 昆明: 昆明医科大学, 2014. [28] LI J, LIU B. More attention to initial surgical treatment of hepatolithiasis[J]. J Clin Hepatol, 2015, 31(10): 1612-1614. DOI: 10.3969/j.issn.1001-5256.2015.10.012.李江, 刘斌. 肝胆管结石初始外科治疗的规范化研究[J]. 临床肝胆病杂志, 2015, 31(10): 1612-1614. DOI: 10.3969/j.issn.1001-5256.2015.10.012. [29] DOS SANTOS JS, JÚNIOR WS, MÓDENA JL, et al. Effect of preoperative endoscopic decompression on malignant biliary obstruction and postoperative infection[J]. Hepatogastroenterology, 2005, 52(61): 45-47. [30] KOSE SH, GRICE K, ORSI WD, et al. Metagenomics of pigmented and cholesterol gallstones: The putative role of bacteria[J]. Sci Rep, 2018, 8(1): 11218. DOI: 10.1038/s41598-018-29571-8. [31] KIM B, PARK JS, BAE J, et al. Bile microbiota in patients with pigment common bile duct stones[J]. J Korean Med Sci, 2021, 36(15): e94. DOI: 10.3346/jkms.2021.36.e94. [32] XIAO Z, HUANG Z, GAO J, et al. The imbalance of biliary microflora in hepatolithiasis[J]. Microb Pathog, 2021, 157: 104966. DOI: 10.1016/j.micpath.2021.104966. [33] HUANG ZQ, YANG KZ, MENG XJ, et al. The significance of bile β-glucuronidase activity[J]. Chin J Surg, 1982, 20(1): 49-52.黄志强, 杨可桢, 孟宪钧, 等. 胆汁β-葡萄糖醛酸酶活性的意义[J]. 中华外科杂志, 1982, 20(1): 49-52. [34] FAN HJ, TIAN DG, WEI XP. Advances in etiological mechanism and surgical treatment of recurrent intrahepatic bile duct stones[J]. Chin J New Clin Med, 2019, 12(9): 1029-1034. DOI: 10.3969/j.issn.1674-3806.2019.09.27.范海军, 田大广, 魏晓平. 复发性肝内胆管结石病因机制及外科治疗究进展[J]. 中国临床新医学, 2019, 12(9): 1029-1034. DOI: 10.3969/j.issn.1674-3806.2019.09.27. [35] YANG L, JUNMIN S, HONG Y, et al. PGE(2) induces MUC2 and MUC5AC expression in human intrahepatic biliary epithelial cells via EP4/p38MAPK activation[J]. Ann Hepatol, 2013, 12(3): 479-486. DOI: 10.1016/S1665-2681(19)31012-9 [36] SHODA J, KANO M, ASANO T, et al. Secretory low-molecular-weight phospholipases A2 and their specific receptor in bile ducts of patients with intrahepatic calculi: Factors of chronic proliferative cholangitis[J]. Hepatology, 1999, 29(4): 1026-1036. DOI: 10.1002/hep.510290440. [37] LI FY, CHENG NS, MAO H, et al. Significance of controlling chronic proliferative cholangitis in the treatment of hepatolithiasis[J]. World J Surg, 2009, 33(10): 2155-2160. DOI: 10.1007/s00268-009-0154-8. [38] ZHANG Z. Detection of Hp infection and its related proteins and β-glucuronidase in gallbladder bile and mucosa in patients with gallbladder stones and its significance[D]. Hefei: Anhui Medical University, 2007.张震. 胆囊结石患者胆囊胆汁、粘膜中Hp感染与其相关蛋白和β-葡萄糖醛酸酶检测及其意义[D]. 合肥: 安徽医科大学, 2007. [39] HAN J, WU S, FAN Y, et al. Biliary microbiota in choledocholithiasis and correlation with duodenal microbiota[J]. Front Cell Infect Microbiol, 2021, 11: 625589. DOI: 10.3389/fcimb.2021.625589. [40] LI T, MENG XL. Pathogenic mechanism of helicobacter pylori in primary intrahepatic stones[J]. Chin J Dig Surg, 2007, 6(1): 58-60. DOI: 10.3760/cma.j.issn.1673-9752.2007.01.021.李霆, 孟翔凌. 幽门螺杆菌与原发性肝内胆管结石的关系[J]. 中华消化外科杂志, 2007, 6(1): 58-60. DOI: 10.3760/cma.j.issn.1673-9752.2007.01.021. [41] ZENG Y, XIAO LJ, YAO HH, et al. A study of the immune in formation of calcium bilirubinate gallstones in different rabbit models-The changes of the immunoglobulins in serum and bile and the immunoglobulins forming cells in the gallbladder mucoderm[J]. J West China Univ Med Sci, 2000, 31(2): 155-158. DOI: 10.3969/j.issn.1672-173X.2000.02.009.曾勇, 肖路加, 姚辉华, 等. 兔胆红素钙结石成石过程中血清、胆汁免疫球蛋白和胆囊免疫球蛋白分泌细胞含量的变化[J]. 华西医大学报, 2000, 31(2): 155-158. DOI: 10.3969/j.issn.1672-173X.2000.02.009. [42] TIAN FZ. Discussion of hepatolithiasis[J]. Clin Misdiagn Misther, 2012, 25(1): 1-4. DOI: 10.3969/j.issn.1002-3429.2012.01.001.田伏洲. 肝内胆结石探索无止境[J]. 临床误诊误治, 2012, 25(1): 1-4. DOI: 10.3969/j.issn.1002-3429.2012.01.001. [43] SUN SL, WU SD, DAI XW, et al. Endotoxin regulates the expression of hepatocyte β-glucuronidase mRNA[J]. World Chin J Dig, 2007, 15(17): 1887-1892. https://www.cnki.com.cn/Article/CJFDTOTAL-XXHB200717006.htm孙韶龙, 吴硕东, 戴显伟, 等. 内毒素调节肝脏β-葡萄糖苷酸酶mRNA的表达[J]. 世界华人消化杂志, 2007, 15(17): 1887-1892. https://www.cnki.com.cn/Article/CJFDTOTAL-XXHB200717006.htm [44] YAO CH. The role of LINC00311 in LPS-induced human intrahepatic bile duct epithelial cells to activate the TLR4/NF-κB/c-myc signaling pathway to up-regulate the expression of endogenous β-glucuronidase[D]. Shenyang: China Medical University, 2019.姚晨辉. LINC00311在LPS诱导人肝内胆管上皮细胞激活TLR4/NF-κB/c-myc信号通路从而上调内源性β-葡萄糖醛酸酶表达过程中的作用[D]. 沈阳: 中国医科大学, 2019. [45] YAO D, DONG Q, TIAN Y, et al. Lipopolysaccharide stimulates endogenous β-glucuronidase via PKC/NF-κB/c-myc signaling cascade: A possible factor in hepatolithiasis formation[J]. Mol Cell Biochem, 2018, 444(1-2): 93-102. DOI: 10.1007/s11010-017-3234-3. [46] MANNE A, ESNAKULA A, ABUSHAHIN L, et al. Understanding the clinical impact of MUC5AC expression on pancreatic ductal adenocarcinoma[J]. Cancers (Basel), 2021, 13(12): 3059. DOI: 10.3390/cancers13123059. [47] GRIGOR'EVA IN, ROMANOVA TI. Gallstone disease and microbiome[J]. Microorganisms, 2020, 8(6): 835. DOI: 10.3390/microorganisms8060835. [48] SHEN Y, CHEN Z, WANG Y, et al. Aquaporin 5 expression inhibited by LPS via p38/JNK signaling pathways in SPC-A1 cells[J]. Respir Physiol Neurobiol, 2010, 171(3): 212-217. DOI: 10.1016/j.resp.2010.03.021. [49] LI M, TIAN Y, WU S, et al. LPS stimulates MUC5AC expression in human biliary epithelial cells: Whether there exists a possible pathway of PKC/NADPH/ROS?[J]. Mol Cell Biochem, 2014, 385(1-2): 87-93. DOI: 10.1007/s11010-013-1817-1. [50] WANG P, MA X, HE Y, et al. Effect of p38 mitogen-activate protein kinase on MUC5AC protein expression of bile duct epithelial cells in hepatolithiasis patients[J]. Int J Clin Exp Pathol, 2015, 8(10): 13753-13758. [51] KHARE A, GAUR S. Cholesterol-lowering effects of lactobacillus species[J]. Curr Microbiol, 2020, 77(4): 638-644. DOI: 10.1007/s00284-020-01903-w. [52] RUIZ L, MARGOLLES A, SÁNCHEZ B. Bile resistance mechanisms in Lactobacillus and Bifidobacterium[J]. Front Microbiol, 2013, 4: 396. DOI: 10.3389/fmicb.2013.00396. [53] YE FQ. Metagenomics study of the biliary tract of patients with common bile duct stones and the intestines of Alzheimer's mice[D]. Beijing: Academy of Military Medical Sciences, 2016.叶福强. 胆总管结石患者胆道和阿尔茨海默症小鼠肠道的宏基因组学研究[D]. 北京: 中国人民解放军军事医学科学院, 2016. [54] VÍTEK L, CAREY MC. New pathophysiological concepts underlying pathogenesis of pigment gallstones[J]. Clin Res Hepatol Gastroenterol, 2012, 36(2): 122-129. DOI: 10.1016/j.clinre.2011.08.010. -



 PDF下载 ( 3084 KB)
PDF下载 ( 3084 KB)


 下载:
下载: