血栓弹力图对肝硬化患者自发性出血风险的评估价值
DOI: 10.3969/j.issn.1001-5256.2021.07.021
Role of thromboelastography in assessing the risk of spontaneous bleeding in patients with liver cirrhosis
-
摘要:
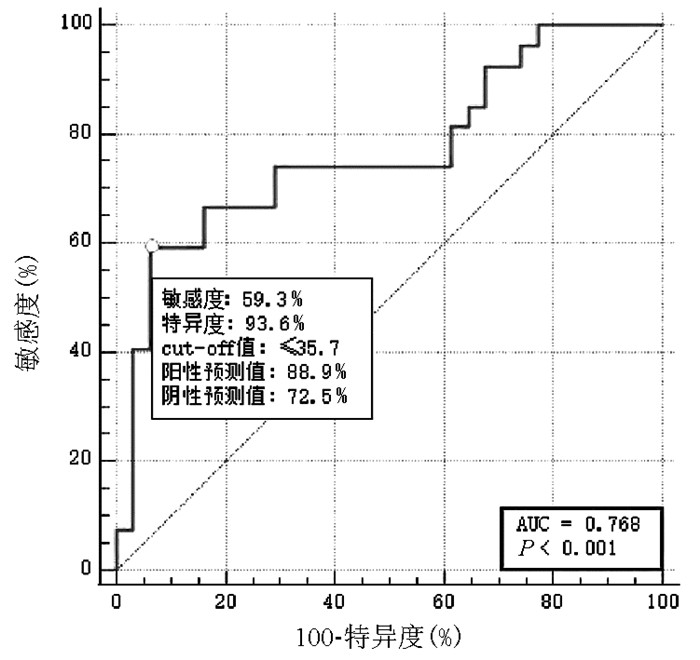
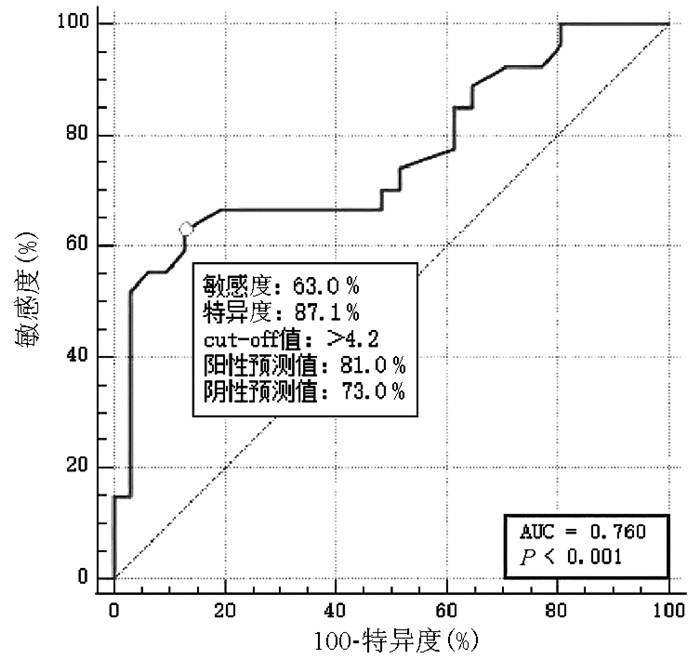
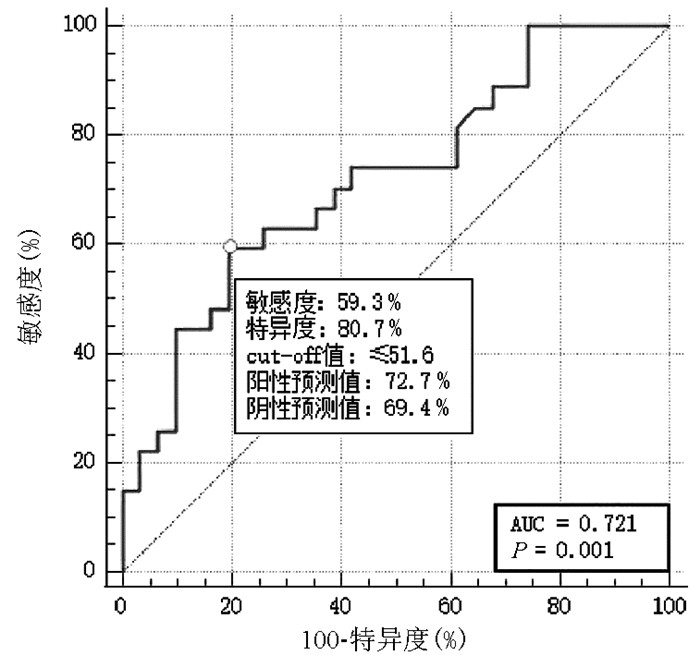
目的 分析肝硬化患者血栓弹力图(TEG)检测结果与出血的关系,探讨TEG是否可以用于肝硬化患者自发性出血风险的预测,为其预防性治疗提供依据。 方法 回顾性分析2018年5月—2020年4月在广州市花都区人民医院就诊的174例无大的侵入性操作的肝硬化患者,根据出血情况分成为未出血组(n=64)、消化道出血组(n=61)和皮肤黏膜及口鼻出血组(n=49),通过病历系统、实验室信息系统等收集患者信息及相应的实验室检测结果进行统计分析。TEG参数包括R(凝血反应时间)、K(血块形成时间)、a角(凝血固定角)、MA(凝血最大幅度)、Lys30(30 min纤溶率)及CI(综合凝血指数),常规凝血指标包括PLT、纤维蛋白原(FIB)、PT、APTT。符合正态分布的计量资料两组比较采用t检验,多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验。非正态分布的计量资料两组间比较采用Mann-Whitney U检验,多组间比较采用Kruskal-Wallis H检验。MedCalc软件进行ROC曲线分析,计算常用凝血试验指标和TEG检测指标预测肝硬化患者出血能力的ROC曲线下面积(AUC),确定标准预测值,敏感度、特异度、阳性预测值和阴性预测值,各检测值对皮肤黏膜及口鼻出血的预测比较采用Z检验。 结果 MA、K在出血组与未出血组组间比较差异均存在统计学意义(t值分别为2.241、-2.605,P值均<0.05)。皮肤黏膜及口鼻出血组、未出血组和消化道出血组3组间PLT及TEG参数K、a角、MA和CI比较有显著性差别(F=3.947、H=12.867、F=4.007、F=8.498、F=5.420,P值均<0.05)。TEG参数中,R、Lys30大多处于正常值之间,K延长,a角、MA和CI下降。当PLT≤40×109/L、MA≤35.7 mm、K值>4.2 min、a角≤51.6和CI≤-5.9可以预测肝硬化患者皮肤黏膜及口鼻自发性出血(AUC均>0.7),其阳性预测值分别为82.4、88.9、81.0、72.7、73.7,阴性预测值分别为68.3、72.5、73.0、69.4、66.7。 结论 PLT和TEG参数K、a角、MA和CI可以预测肝硬化凝血异常导致的自发性出血,常规凝血试验PT和APTT异常不能,为肝硬化患者凝血异常的治疗及血液成分输注提供依据。 Abstract:Objective To investigate the association between thromboelastography (TEG) parameters and bleeding in patients with liver cirrhosis and whether TEG can be used to predict the risk of spontaneous bleeding in patients with liver cirrhosis, and to provide a basis for its preventive treatment. Methods A retrospective analysis was performed for the clinical data of 174 patients with liver cirrhosis who attended Huadu People's Hospital from May 2018 to April 2020 and did not receive invasive procedure, and according to the condition of bleeding, they were divided into non-bleeding group(n=64), gastrointestinal bleeding group(n=61), and mucocutaneous/oronasal bleeding group(n=49). The medical record system and laboratory information system were used to collect related information and laboratory test results for statistical analysis. The t-test was used for comparison of normally distributed continuous data between two groups; an analysis of variance was used for comparison between multiple groups, and the least significant difference t-test was used for further comparison between two groups. The Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between multiple groups. MedCalc software was used for receiver operating characteristic (ROC) curve analysis, and the area under the ROC curve (AUC) was calculated for commonly used coagulation markers and TEG parameters in predicting the risk of bleeding in patients with liver cirrhosis. Cut-off value, sensitivity, specificity, positive predictive value, and negative predictive value were determined, and the Z test was used for comparison of indices in predicting mucocutaneous/oronasal bleeding. Results Of all 174 patients, 110 (63.2%) experienced spontaneous bleeding, among whom 61 (55.5%) had gastrointestinal bleeding and 49 (44.5%) had mucocutaneous/oronasal bleeding. There were significant differences in maximum amplitude (MA) and K between the bleeding group and the non-bleeding group (t=2.241 and -2.605, both P < 0.05). There were significant differences between the mucocutaneous/oronasal bleeding group and the non-bleeding/gastrointestinal bleeding groups in platelet count (PLT) and the TEG parameters of clot formation time, a-angle, MA, and coagulation index (CI) (F=3.947, H=12.867, F=4.007, F=8.498, F=5.420, all P < 0.05). Among the TEG parameters, reaction time and Lys30 were generally within the normal range, while there was a prolonged kinetics (K) time and reductions in a-angle, MA, and CI. PLT ≤40×109/L, MA ≤35.7 mm, K time > 4.2 minutes, a-angle ≤51.6, and CI ≤-5.9 could be used to predict spontaneous mucocutaneous/oronasal bleeding in patients with liver cirrhosis (all AUC > 0.7), with positive predictive values of 82.4, 88.9, 81.0, 72.7, and 73.7, respectively, and negative predictive values of 68.3, 72.5, 73.0, 69.4, and 66.7, respectively. Conclusion PLT and the TEG parameters of K time, a-angle, MA, and CI can predict spontaneous bleeding caused by abnormal coagulation in liver cirrhosis, while conventional coagulation parameters prothrombin time and activated partial thromboplastin time cannot predict such bleeding, which provides a basis for the treatment of coagulation disorder and transfusion of blood components for patients with liver cirrhosis. -
Key words:
- Thromboelastography /
- Liver Cirrhosis /
- Hemorrhage
-
表 1 174例肝硬化患者基本特征
参数 数值 年龄(岁) 58(45~66) 男/女(例) 109/65 MELD评分(分) 20.6(15.3~27.3) Child-Pugh评分(分) 11.0(9.3~12.0) Child-Pugh分级[例(%)] A级 8(4.6) B级 38(21.8) C级 128(73.6) 出血情况[例(%)] 未出血 64(36.8) 消化道出血 61(35.1) 皮肤黏膜及口鼻出血 49(28.2) 临床生化 血红蛋白(mg/L) 88(72~111) TBil(μmol/L) 150.0(52.4~315.7) 白蛋白(g/L) 27.4(24.3~31.1) ALT(U/L) 48.3(25.1~173.2) AST(U/L) 73.1(44.8~255.2) 肌酐(μmol/L) 69.3(55.5~109.6) 表 2 肝病患者TEG参数与常规凝血指标结果
指标 例数 数值 正常值 >正常值[例(%)] 正常值之间[例(%)] <正常值[例(%)] TEG参数 R(min) 174 5.96±1.37 5~10 11(6.3) 121(69.5) 42(24.1) K(min) 168 3.40(2.30~5.25) 1~3 93(55.4) 75(44.6) 0 a角 174 53.78±12.38 53~72 7(4.0) 96(55.2) 71(40.8) MA(mm) 174 40.88±11.27 50~70 2(1.1) 30(17.2) 142(81.6) Lys30 174 0.10(0.10~0.10) 0~8 1(0.6) 173(99.4) 0 CI 168 -4.30±3.73 -3~3 0 65(38.7) 103(61.3) 常规凝血指标 PLT(×109/L) 174 88.24±60.80 100~300 0 54(31.0) 120(69.0) FIB(g/L) 174 1.63±0.69 2~4 3(1.7) 36(20.7) 135(77.6) PT(s) 174 23.7(19.8~27.3) 11.0~14.5 172(98.9) 2(1.1) 0 APTT(s) 174 53.8±16.76 28~40 154(88.5) 19(10.9) 1(0.6) 表 3 出血组与未出血组间TEG及常规实验室检测指标比较
指标 未出血(n=64) 出血组(n=110) 统计值 P值 PLT(×109/L) 101.03±66.29 81.02±56.77 t=1.568 0.120 FIB(g/L) 1.77±0.82 1.55±0.61 t=1.487 0.140 PT(s) 26.05(20.20~28.20) 23.25(19.50~26.40) Z=-1.345 0.179 APTT(s) 53.16±10.46 54.15±19.45 t=-0.275 0.784 R(min) 6.15±1.47 5.86±1.33 t=0.986 0.326 K(min) 3.53±2.21 5.20±4.08 t=-2.605 0.011 a角 56.72±9.85 52.80±12.25 t=1.622 0.108 MA(mm) 44.63±11.89 39.30±10.86 t=2.241 0.027 Lys30 0.40±0.71 0.19±0.44 t=1.542 0.129 CI -3.37±3.15 -4.82±3.95 t=1.867 0.065 表 4 不同出血组与无出血组TEG及常规实验室检测指标比较
指标 未出血组(n=64) 消化道出血组(n=61) 皮肤黏膜及口鼻出血组(n=49) 统计值 P值 PLT(×109/L) 101.03±66.29 100.07±65.38 65.32±43.571)2) F=3.947 0.023 FIB(g/L) 1.77±0.82 1.59±0.77 1.52±0.44 F=1.155 0.319 PT(s) 26.05(20.2~28.2) 22.25(18.15~26.23) 23.85(20.48~26.48) H=2.447 0.294 APTT(s) 53.16±10.46 52.95±26.92 55.14±10.21 F=0.166 0.848 R(min) 6.15±1.47 5.95±1.40 5.78±1.28 F=0.604 0.549 K(min) 3.40(2.00~4.20) 2.90(1.90~4.55) 5.00(2.98~7.40)1)2) H=12.867 0.002 a角 56.72±9.85 56.39±12.53 49.83±11.371)2) F=4.007 0.021 MA(mm) 44.63±11.89 44.34±10.97 35.14±8.96 1)2) F=8.498 <0.001 Lys30 0.10(0.10~0.15) 0.10(0.10~0.10) 0.10(0.10~0.10) H=4.172 0.124 CI -3.37±3.15 -3.49±3.62 -5.92±3.921)2) F=5.420 0.006 注:与未出血组比较,1)P<0.05;与消化道出血组比较,2)P<0.05。 表 5 TEG参数和常规检测指标预测皮肤黏膜及口鼻出血AUC
指标 标准误 AUC 95%CI R 0.078 0.576 0.424~0.728 a角 0.068 0.721 0.582~0.849 K 0.066 0.760 0.630~0.860 MA 0.065 0.768 0.631~0.890 Lys30 0.075 0.610 0.464~0.757 CI 0.067 0.725 0.591~0.853 PLT 0.069 0.713 0.566~0.840 INR 0.078 0.572 0.419~0.725 APTT 0.078 0.476 0.324~0.628 FIB 0.079 0.514 0.360~0.668 -
[1] LISMAN T, PORTE RJ. Rebalanced hemostasis in patients with liver disease: Evidence and clinical consequences[J]. Blood, 2010, 116(6): 878-885. DOI: 10.1182/blood-2010-02-261891. [2] TRIPODI A, MANNUCCI PM. The coagulopathy of chronic liver disease[J]. N Engl J Med, 2011, 365(2): 147-156. DOI: 10.1056/NEJMra1011170. [3] LISMAN T, PORTE RJ. Value of preoperative hemostasis testing in patients with liver disease for perioperative hemostatic management[J]. Anesthesiology, 2017, 126(2): 338-344. DOI: 10.1097/ALN.0000000000001467. [4] PEI DC, ZHENG JX, WEN SS, et al. Analysis of fresh frozen plasma use in liver disease[J]. Lab Med Clin, 2018, 15(23): 3590-3593. DOI: 10.3969/j.issn.1672-9455.2018.23.033.裴德翠, 郑金秀, 文思思, 等. 肝病患者新鲜冰冻血浆输注情况分析[J]. 检验医学与临床, 2018, 15(23): 3590-3593. DOI: 10.3969/j.issn.1672-9455.2018.23.033. [5] NOGAMI K. The utility of thromboelastography in inherited and acquired bleeding disorders[J]. Br J Haematol, 2016, 174(4): 503-514. DOI: 10.1111/bjh.14148. [6] STRAVITZ RT. Potential applications of thromboelastography in patients with acute and chronic liver disease[J]. Gastroenterol Hepatol (N Y), 2012, 8(8): 513-520. https://pubmed.ncbi.nlm.nih.gov/23293564/ [7] DEBERNARDI VENON W, PONZO P, SACCO M, et al. Usefulness of thromboelastometry in predicting the risk of bleeding in cirrhotics who undergo invasive procedures[J]. Eur J Gastroenterol Hepatol, 2015, 27(11): 1313-1319. DOI: 10.1097/MEG.0000000000000442. [8] SOMANI V, AMARAPURKAR D, SHAH A. Thromboelastography for assessing the risk of bleeding in patients with cirrhosis-moving closer[J]. J Clin Exp Hepatol, 2017, 7(4): 284-289. DOI: 10.1016/j.jceh.2017.03.001. [9] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [10] GIANNINI EG, STRAVITZ RT, CALDWELL SH. Correction of hemostatic abnormalities and portal pressure variations in patients with cirrhosis[J]. Hepatology, 2014, 60(4): 1442. DOI: 10.1002/hep.27029. [11] DELANEY M, WENDEL S, BERCOVITZ RS, et al. Transfusion reactions: Prevention, diagnosis, and treatment[J]. Lancet, 2016, 388(10061): 2825-2836. DOI: 10.1016/S0140-6736(15)01313-6. [12] de PIETRI L, BIANCHINI M, ROMPIANESI G, et al. Thromboelastographic reference ranges for a cirrhotic patient population undergoing liver transplantation[J]. World J Transplant, 2016, 6(3): 583-593. DOI: 10.5500/wjt.v6.i3.583. [13] LLOYD-DONALD P, VASUDEVAN A, ANGUS P, et al. Coagulation in acutely ill patients with severe chronic liver disease: Insights from thromboelastography[J]. J Crit Care, 2017, 38: 215-224. DOI: 10.1016/j.jcrc.2016.10.030. [14] SHAMSEDDEEN H, PATIDAR KR, GHABRIL M, et al. Features of blood clotting on thromboelastography in hospitalized patients with cirrhosis[J]. Am J Med, 2020, 133(12): 1479-1487. e2. DOI: 10.1016/j.amjmed.2020.04.029. [15] KLEINEGRIS MC, BOS MH, ROEST M, et al. Cirrhosis patients have a coagulopathy that is associated with decreased clot formation capacity[J]. J Thromb Haemost, 2014, 12(10): 1647-1657. DOI: 10.1111/jth.12706. [16] LEEBEEK FW, RIJKEN DC. The fibrinolytic status in liver diseases[J]. Semin Thromb Hemost, 2015, 41(5): 474-480. DOI: 10.1055/s-0035-1550437. [17] LISMAN T, CALDWELL SH, BURROUGHS AK, et al. Hemostasis and thrombosis in patients with liver disease: The ups and downs[J]. J Hepatol, 2010, 53(2): 362-371. DOI: 10.1016/j.jhep.2010.01.042. [18] INTAGLIATA NM, DAVIS J, CALDWELL SH. Coagulation pathways, hemostasis, and thrombosis in liver failure[J]. Semin Respir Crit Care Med, 2018, 39(5): 598-608. DOI: 10.1055/s-0038-1673658. [19] MA JL, HE LL, JIANG Y, et al. New model predicting gastroesophageal varices and variceal hemorrhage in patients with chronic liver disease[J]. Ann Hepatol, 2020, 19(3): 287-294. DOI: 10.1016/j.aohep.2019.12.007. [20] DUAN ZH, ZHOU SY, LI ZK, et al. Value of platelet count-to-gallbladder wall thickness ratio score in predicting esophageal varices in patients with liver cirrhosis[J]. J Clin Hepatol, 2019, 35(12): 2716-2720. DOI: 10.3969/j.issn.1001-5256.2019.12.015.段志辉, 周胜云, 李增魁, 等. 血小板计数/胆囊壁厚度对肝硬化食管静脉曲张的预测价值[J]. 临床肝胆病杂志, 2019, 35(12): 2716-2720. DOI: 10.3969/j.issn.1001-5256.2019.12.015. [21] STOTTS MJ, DAVIS J, SHAH NL. Coagulation testing and management in liver disease patients[J]. Curr Opin Gastroenterol, 2020, 36(3): 169-176. DOI: 10.1097/MOG.0000000000000635. [22] BIHARI C, PATIL A, SHASTHRY SM, et al. Viscoelastic test-based bleeding risk score reliably predicts coagulopathic bleeding in decompensated cirrhosis and ACLF patients[J]. Hepatol Int, 2020, 14(4): 597-608. DOI: 10.1007/s12072-020-10036-y. [23] LISMAN T, ARIËNS RA. Alterations in fibrin structure in patients with liver diseases[J]. Semin Thromb Hemost, 2016, 42(4): 389-396. DOI: 10.1055/s-0036-1572327. [24] GIANNINI EG, GIAMBRUNO E, BRUNACCI M, et al. Low fibrinogen levels are associated with bleeding after varices ligation in thrombocytopenic cirrhotic patients[J]. Ann Hepatol, 2018, 17(5): 830-835. DOI: 10.5604/01.3001.0012.0775. [25] TAPPER EB, ROBSON SC, MALIK R. Coagulopathy in cirrhosis-the role of the platelet in hemostasis[J]. J Hepatol, 2013, 59(4): 889-890. DOI: 10.1016/j.jhep.2013.03.040. [26] WITTERS P, FRESON K, VERSLYPE C, et al. Review article: Blood platelet number and function in chronic liver disease and cirrhosis[J]. Aliment Pharmacol Ther, 2008, 27(11): 1017-1029. DOI: 10.1111/j.1365-2036.2008.03674.x. [27] THAKRAR SV, MALLETT SV. Thrombocytopenia in cirrhosis: Impact of fibrinogen on bleeding risk[J]. World J Hepatol, 2017, 9(6): 318-325. DOI: 10.4254/wjh.v9.i6.318. [28] LAWSON PJ, MOORE HB, MOORE EE, et al. Preoperative thrombelastography maximum amplitude predicts massive transfusion in liver transplantation[J]. J Surg Res, 2017, 220: 171-175. DOI: 10.1016/j.jss.2017.05.115. [29] PREMKUMAR M, SAXENA P, RANGEGOWDA D, et al. Coagulation failure is associated with bleeding events and clinical outcome during systemic inflammatory response and sepsis in acute-on-chronic liver failure: An observational cohort study[J]. Liver Int, 2019, 39(4): 694-704. DOI: 10.1111/liv.14034. [30] KUMAR M, AHMAD J, MAIWALL R, et al. Thromboelastography-guided blood component use in patients with cirrhosis with nonvariceal bleeding: A randomized controlled trial[J]. Hepatology, 2020, 71(1): 235-246. DOI: 10.1002/hep.30794. -



 PDF下载 ( 2243 KB)
PDF下载 ( 2243 KB)


 下载:
下载: