| [1] |
Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019)[J]. J Clin Hepatol, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. |
| [2] |
YE J, WANG W, FENG S, et al. Precise fibrosis staging with shear wave elastography in chronic hepatitis B depends on liver inflammation and steatosis[J]. Hepatol Int, 2020, 14(2): 190-201. DOI: 10.1007/s12072-020-10017-1. |
| [3] |
CHANG JW, LEE HW, KIM BK, et al. Hepatic steatosis index in the detection of fatty liver in patients with chronic hepatitis B receiving antiviral therapy[J]. Gut Liver, 2021, 15(1): 117-127. DOI: 10.5009/gnl19301. |
| [4] |
CHEN YC, JENG WJ, HSU CW, et al. Impact of hepatic steatosis on treatment response in nuclesos(t)ide analogue-treated HBeAg-positive chronic hepatitis B: A retrospective study[J]. BMC Gastroenterol, 2020, 20(1): 146. DOI: 10.1186/s12876-020-01289-w. |
| [5] |
GUO Z, BLAKE GM, LI K, et al. Liver fat content measurement with quantitative CT validated against MRI proton density fat fraction: A prospective study of 400 healthy volunteers[J]. Radiology, 2020, 294(1): 89-97. DOI: 10.1148/radiol.2019190467. |
| [6] |
GANDHA N, WIBAWA LP, JACOEB T, et al. Correlation between psoriasis severity and nonalcoholic fatty liver disease degree measured using controlled attenuation parameter[J]. Psoriasis (Auckl), 2020, 10: 39-44. DOI: 10.2147/PTT.S272286. |
| [7] |
MA LX, ZHANG YH, SU BL. Evaluation of liver steatosis and fibrosis in patients of type 2 diabetes mellitus and correlation between liver steatosis and fibrosis by FibroTouch technique[J]. J Chin Clin Med Imaging, 2018, 29(9): 636-639. DOI: 10.12117/jccmi.2018.09.008. |
| [8] |
VITEL A, SPOREA I, MARE R, et al. Association between subclinical left ventricular myocardial systolic dysfunction detected by strain and strain-rate imaging and liver steatosis and fibrosis detected by elastography and controlled attenuation parameter in patients with metabolic syndrome[J]. Diabetes Metab Syndr Obes, 2020, 13: 3749-3759. DOI: 10.2147/DMSO.S268916. |
| [9] |
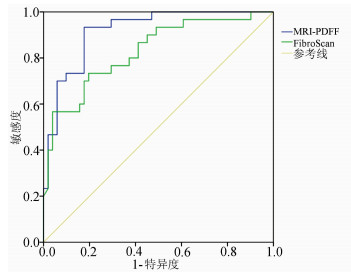
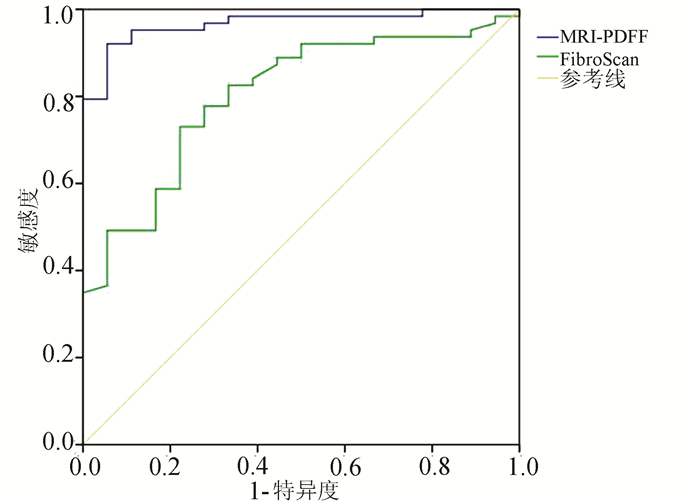
GU Q, CEN L, LAI J, et al. A meta-analysis on the diagnostic performance of magnetic resonance imaging and transient elastography in nonalcoholic fatty liver disease[J]. Eur J Clin Invest, 2021, 51(2): e13446. DOI: 10.1111/eci.13446. |
| [10] |
OEDA S, TANAKA K, OSHIMA A, et al. Diagnostic accuracy of fibroscan and factors affecting measurements[J]. Diagnostics (Basel), 2020, 10(11): 940. DOI: 10.3390/diagnostics10110940. |
| [11] |
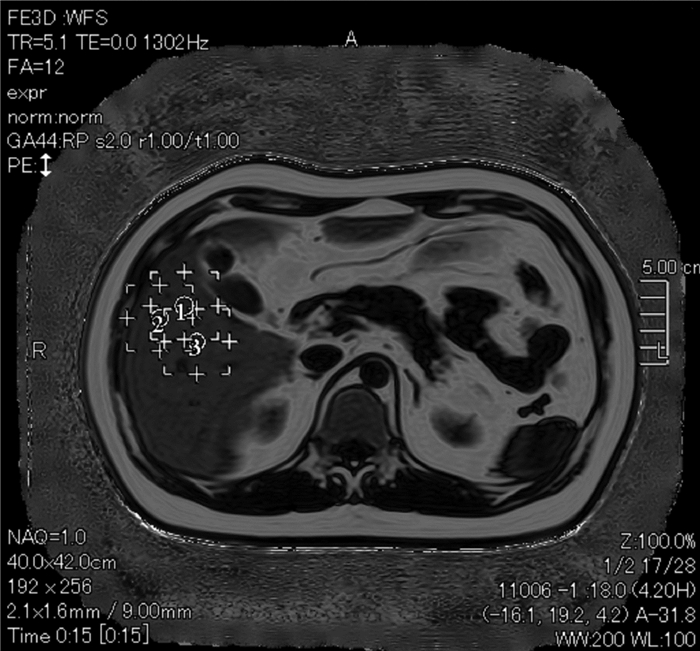
YANG YM, LIU YP, ZHOU DJ, et al. Values of 3.0T MRI PDFF and IP-OP in quantificative evaluation on fatty liver[J]. J Jilin Univ(Med Edit), 2020, 46(4): 875-880. DOI: 10.13481/j.1671-587x.20200434. |
| [12] |
ZHOU DJ, HUANG LX, LIU YP, et al. Value of fatty liver disease by 3.0 T magnetic resonance IDEAL-IQ sequence: A quantitative assessment[J]. Chin J Biomed Eng, 2017, 23(1): 55-58. DOI: 10.3760/cma.j.issn.1674-1927.2017.01.013. |
| [13] |
YE J, WU Y, LI F, et al. Effect of orlistat on liver fat content in patients with nonalcoholic fatty liver disease with obesity: Assessment using magnetic resonance imaging-derived proton density fat fraction[J]. Therap Adv Gastroenterol, 2019, 12: 1756284819879047. DOI: 10.1177/1756284819879047. |
| [14] |
ZHAO S, LIU MW, LIU SF, et al. IDEAL-IQ and CT quantitative analysis for accurate quantitative fat content in nonalcoholic fatty liver disease[J]. J Med Imaging, 2019, 29(12): 2162-2166. DOI: 1006-9011(2019) 12-2162-04.
赵森, 刘梦雯, 刘双锋, 等. 磁共振IDEAL-IQ技术和CT定量分析在非酒精性脂肪肝病的临床应用[J]. 医学影像学杂志, 2019, 29(12): 2162-2166. DOI: 1006-9011(2019) 12-2162-04.
|
| [15] |
GU Q, CEN L, LAI J, et al. A meta-analysis on the diagnostic performance of magnetic resonance imaging and transient elastography in nonalcoholic fatty liver disease[J]. Eur J Clin Invest, 2021, 51(2): e13446. DOI: 10.1111/eci.13446. |






 DownLoad:
DownLoad: