双重血浆分子吸附系统模式人工肝治疗中低血压发生的影响因素分析
DOI: 10.3969/j.issn.1001-5256.2022.09.024
Influencing factors for hypotension in patients undergoing double plasma molecular adsorption system artificial liver support therapy
-
摘要:
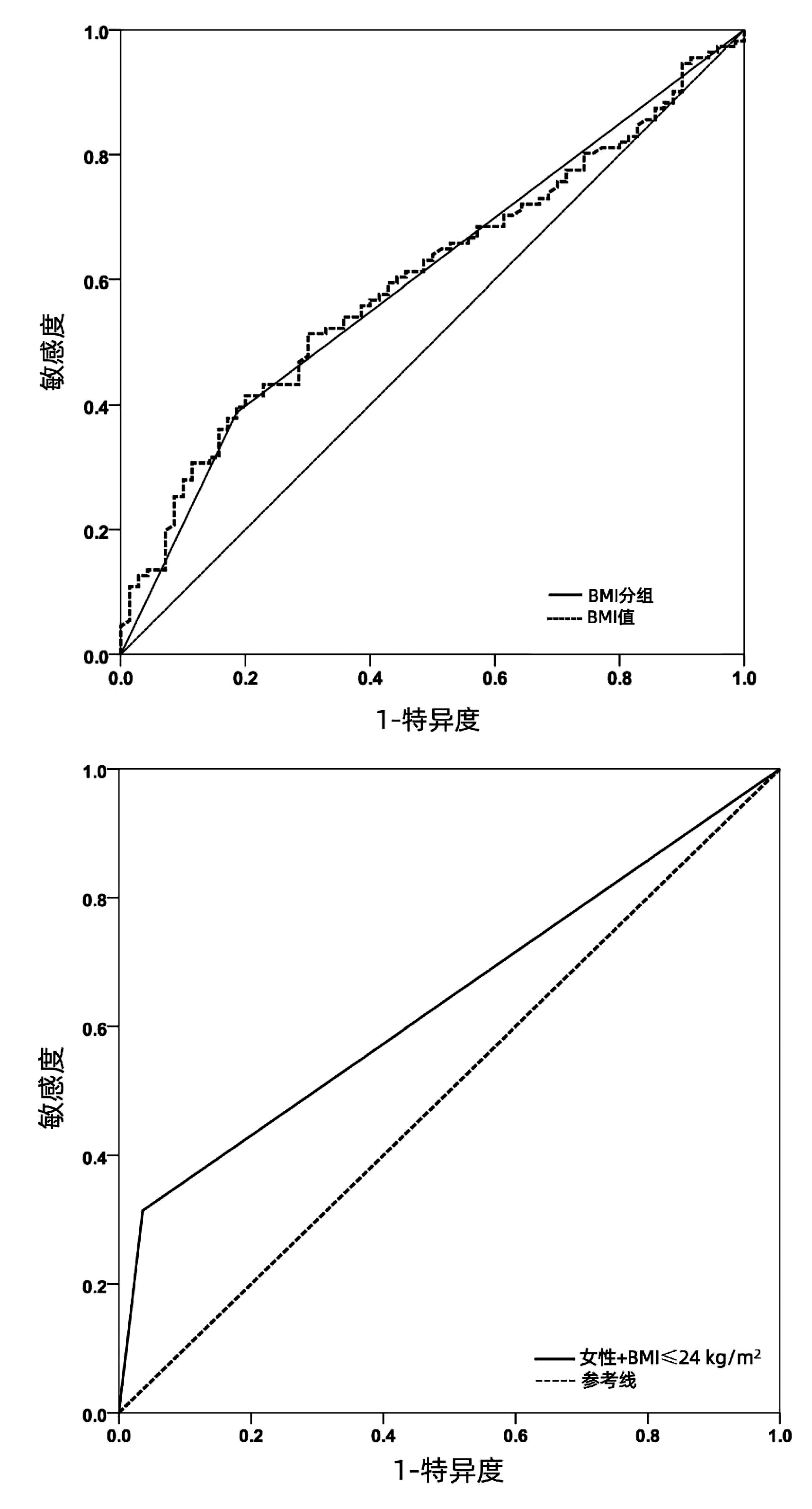
目的 探讨双重血浆分子吸附系统(DPMAS)模式人工肝治疗过程中患者发生低血压(IOH)的相关危险因素。 方法 收集2017年10月1日-2020年12月31日中国科学技术大学附属第一医院肝病中心行DPMAS人工肝治疗的181例患者(共计670例次)的临床资料, 根据人工肝治疗过程中是否发生低血压, 分为IOH组(70例)和非IOH组(111例)。比较两组患者各项临床指标, 并分析其与IOH发生的相关性以及12周、24周预后。符合正态分布的计量资料两组间比较采用独立样本t检验, 非正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料组间比较采用χ2检验。IOH相关危险因素采用单因素及多因素Logistic回归分析。Kaplan-Meier法绘制受试者工作特征曲线(ROC曲线), 独立危险因素的ROC曲线下面积(AUC)比较采用Z检验。 结果 单因素Logistic回归分析显示, 女性、年龄≥50岁、正常及低BMI (≤24 kg/m2)者发生IOH的风险更高(P值均 < 0.05);多因素分析显示, 正常及低BMI (OR=3.290, 95% CI: 1.523~7.108, P=0.002)、女性(OR=5.146, 95% CI: 2.316~11.432, P < 0.001)是DPMAS人工肝患者出现IOH的独立危险因素。女性+BMI≤24 kg/m2联合进行ROC曲线分析, 其预测IOH的AUC为0.639(P=0.002)。IOH组与非IOH组12周(76.53% vs 55.77%, χ2=6.887, P=0.009)和24周(74.49% vs 50.00%, χ2=9.080, P=0.003)的生存率比较差异均有统计学意义。 结论 女性、正常或低BMI值患者行DPMAS模式人工肝治疗中发生低血压风险大; 发生IOH者24周生存预后差。 Abstract:Objective To investigate the risk factors for intraoperative hypotension (IOH) in patients undergoing double plasma molecular adsorption system (DPMAS) artificial liver support therapy. Methods Clinical data were collected from 181 patients (670 cases in total) who underwent DPMAS artificial liver support therapy in Liver Disease Center of The First Affiliated Hospital of University of Science and Technology of China from October 1, 2017 to December 31, 2020, and according to the presence or absence of IOH during DPMAS therapy, they were divided into IOH group with 70 patients and non-IOH group with 111 patients.Clinical indicators were compared between the two groups and their association with IOH was analyzed; prognosis was analyzed at 12 and 24 weeks.The independent samples t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between groups; the chi-square test was used for comparison of categorical data between groups.Univariate and multivariate Logistic regression analyses were used to investigate the risk factors for IOH.The Kaplan-Meier method was used to plot receiver operating characteristic (ROC) curves, and the Z test was used for comparison of the area under the ROC curve (AUC) of independent risk factors. Results The univariate Logistic regression analysis showed that female individuals, individuals aged ≥50 years, and individuals with normal or low body mass index (BMI) tended to have a higher risk of IOH (all P < 0.05), and the multivariate analysis showed that normal or low BMI (odds ratio [OR]=3.290, 95% confidence interval [CI]: 1.523-7.108, P=0.002) and female sex (OR=5.146, 95% CI: 2.316-11.432, P < 0.001) were independent risk factor for IOH in patients undergoing DPMAS artificial liver support therapy.The ROC curve analysis of female sex+BMI ≤24 kg/m2 showed that it had an AUC of 0.639 in predicting IOH (P=0.002).The patients experiencing IOH had a 12-week survival rate of 55.77%(29/52) and a 24-week survival rate of 50%(26/52), and there were significant differences between the two groups in 12-and 24-week survival rates (12-week: 76.53% vs 55.77%, χ2=6.887, P=0.009;24-week: 74.49% vs 50.00%, χ2=9.080, P=0.003). Conclusion The risk of hypotension was higher in female patients and that with normal or low BMI during DPMAS artificial liver therapy.Patients with IOH had poor survival prognosis at 24 weeks after DPMAS therapy. -
Key words:
- Liver, Artificial /
- Hypotension /
- Prognosis
-
表 1 IOH组和非IOH组患者的一般临床资料
Table 1. General information of patients in IOH and non-IOH groups
指标 非IOH组(n=111) IOH组(n=70) 统计值 P值 性别[例(%)] χ2=16.424 <0.001 男 98(88.29) 44(62.86) 女 13(11.71) 26(37.14) 心血管疾病[例(%)] 1(0.90) 0 χ2=0.634 0.426 年龄(岁) 46.38±12.52 51.59±11.61 t=-2.848 0.005 BMI(kg/m2) 22.89±4.15 21.42±3.10 t=2.709 0.007 血红蛋白(g/L) 120.63±21.93 110.91±21.96 t=2.902 0.004 白蛋白(g/L) 32.77±4.03 32.91±4.65 t=-0.210 0.834 总胆红素(μmol/L) 375.88±130.50 391.66±138.15 t=-0.774 0.440 凝血酶原活动度(%) 50.49±32.13 44.35±26.94 t=1.331 0.185 血钠(mmol/L) 136(132~137) 135(130~137) Z=-2.039 0.041 肌酐(μmol/L) 61(49~78) 63(54~86) Z=-0.855 0.392 血糖(mmol/L) 5.13(4.29~7.51) 5.02(4.29~6.63) Z=-0.424 0.672 表 2 IOH发生的单因素Logistic回归分析
Table 2. Univariate Logistic regression analysis of IOH ocurrence
参数 β值 SE Wald χ2值 P值 OR 年龄(≥50岁) 0.688 0.311 4.912 0.027 1.990 BMI(≤24 kg/m2) 1.020 0.364 7.853 0.005 2.773 女性 1.494 0.385 15.048 <0.001 4.455 表 3 IOH发生的多因素Logistic回归分析
Table 3. Multivariate Logistic regression analysis of IOH ocurrence
参数 β值 SE Wald χ2值 P值 OR 95%CI BMI(≤24 kg/m2) 1.191 0.393 9.183 0.002 3.290 1.523~7.108 女性 1.638 0.407 16.179 <0.001 5.146 2.316~11.432 -
[1] PALMER BF, HENRICH WL. Recent advances in the prevention and management of intradialytic hypotension[J]. J Am Soc Nephrol, 2008, 19(1): 8-11. DOI: 10.1681/ASN.2007091006. [2] HU D, WU XF, TU WP. Recent advances in clinical research of intradialytic hypotension[J]. Chin Gen Prac, 2017, 20(6): 759-762. DOI: 10.3969/j.issn.1007-9572.2017.06.026.胡丹, 吴险峰, 涂卫平. 血液透析相关性低血压的临床研究进展[J]. 中国全科医学, 2017, 20(6): 759-762. DOI: 10.3969/j.issn.1007-9572.2017.06.026. [3] SHEN TT, FU CZ. Effects of intraoperative hypotension on vital organ function and prognosis in patients undergoing surgery[J]. Int J Anesth Resus, 2017, 38(8): 741-746. DOI: 10.3760/cma.j.issn.1673-4378.2017.08.016.沈通桃, 傅诚章. 术中低血压对手术患者重要器官功能和预后的影响[J]. 国际麻醉学与复苏杂志, 2017, 38(8): 741-746. DOI: 10.3760/cma.j.issn.1673-4378.2017.08.016. [4] NIAN SJ. Research progress on prevention of intradialysis hypotension in diabetic nephropathy patients on maintenant hemodialysis[J]. Zhejiang Med J, 2017, 39(3): 228-231. DOI: 10.3760/cma.j.issn.1673-4378.2017.08.016.年素娟. 预防维持性血液透析糖尿病肾病患者透析中低血压的研究进展[J]. 浙江医学, 2017, 39(3): 228-231. DOI: 10.3760/cma.j.issn.1673-4378.2017.08.016. [5] JIAO ZF, ZHANG YM, MA XF, et al. Effects of different ultrafiltration rates on the incidence of hypotension and cardiovascular death in patients with diabetes nephropathy during maintenance hemodialysis[J]. Clin J Med Offic, 2021, 49(9): 1002-1004. DOI: 10.16680/j.1671-3826.2021.09.14.焦占峰, 张宜明, 马小芬, 等. 不同超滤率对糖尿病肾病患者维持性血液透析中低血压及心血管死亡发生率影响[J]. 临床军医杂志, 2021, 49(9): 1002-1004. DOI: 10.16680/j.1671-3826.2021.09.14. [6] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [7] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association. Guideline for non-bioartificial liver support systems in treatment of liver failure: 2016 update[J]. Chin J Clin Infect Dis, 2016, 9(2): 97-103. DOI: 10.3760/cma.j.issn.1674-2397.2016.02.001.中华医学会感染病学分会肝衰竭与人工肝学组. 非生物型人工肝治疗肝衰竭指南(2016年版)[J]. 中华临床感染病杂志, 2016, 9(2): 97-103. DOI: 10.3760/cma.j.issn.1674-2397.2016.02.001. [8] SANDS JJ, USVYAT LA, SULLIVAN T, et al. Intradialytic hypotension: frequency, sources of variation and correlation with clinical outcome[J]. Hemodial Int, 2014, 18(2): 415-422. DOI: 10.1111/hdi.12138. [9] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33(10): 1847-1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33(10): 1847-1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [10] TANDON P, NEY M, IRWIN I, et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value[J]. Liver Transpl, 2012, 18(10): 1209-1216. DOI: 10.1002/lt.23495. [11] OBI Y, RHEE CM, MATHEW AT, et al. Residual kidney function decline and mortality in incident hemodialysis patients[J]. J Am Soc Nephrol, 2016, 27(12): 3758-3768. DOI: 10.1681/ASN.2015101142. [12] CHANG TI, PAIK J, GREENE T, et al. Intradialytic hypotension and vascular access thrombosis[J]. J Am Soc Nephrol, 2011, 22(8): 1526-1533. DOI: 10.1681/ASN.2010101119. [13] RITZ E. Left ventricular hypertrophy in renal disease: beyond preload and afterload[J]. Kidney Int, 2009, 75(8): 771-773. DOI: 10.1038/ki.2009.35. [14] MALIK J, LACHMANOVA J, KUDLICKA J, et al. Left atrial dysfunction in end-stage renal disease patients treated by hemodialysis[J]. Nephron, 2016, 133(3): 169-174. DOI: 10.1159/000447500. [15] STEFÁNSSON BV, BRUNELLI SM, CABRERA C, et al. Intradialytic hypotension and risk of cardiovascular disease[J]. Clin J Am Soc Nephrol, 2014, 9(12): 2124-2132. DOI: 10.2215/CJN.02680314. [16] LI YY, ZHU HD. Analysis of risk factors of intradialytic hypotension and its correlation with death[J/CD]. Chin J Front Med Sci (Electronic Version), 2019, 11(12): 106-109. DOI: 10.12037/YXQY.2019.12-15.李媛媛, 祝浩栋. 透析中低血压的危险因素及其与患者死亡的相关性分析[J/CD]. 中国医学前沿杂志(电子版), 2019, 11(12): 106-109. DOI: 10.12037/YXQY.2019.12-15. [17] KUIPERS J, VERBOOM LM, IPEMA K, et al. The prevalence of intradialytic hypotension in patients on conventional hemodialysis: A systematic review with meta-analysis[J]. Am J Nephrol, 2019, 49(6): 497-506. DOI: 10.1159/000500877. [18] EL AMRANI M, EL KABBAJ D. Isolated diastolic hypotension in hemodialysis: Risk factor for novel cardiovascular complications and all-cause mortality[J]. Ann Cardiol Angeiol (Paris), 2019, 68(3): 144-149. DOI: 10.1016/j.ancard.2018.09.010. [19] HALLE MP, HILAIRE D, FRANCOIS KF, et al. Intradialytic hypotension and associated factors among patients on maintenance hemodialysis: A single-center study in cameroon[J]. Saudi J Kidney Dis Transpl, 2020, 31(1): 215-223. DOI: 10.4103/1319-2442.279944. [20] LI Y, WRIGHT MD. Patient positioning during a hypotensive episode for adults undergoing hemodialysis: A review of clinical effectiveness and guidelines[M]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health, 2020. [21] WANG Y, JIANG Y, ZHANG M, et al. Prevalence and relevant factors of adult hypoteusion in China[J]. Pract Prev Med, 2009, 16(1): 49-51. DOI: 10.3969/j.issn.1006-3110.2009.01.016.汪媛, 姜勇, 张梅, 等. 中国成人低血压患病率及其相关因素[J]. 实用预防医学, 2009, 16(1): 49-51. DOI: 10.3969/j.issn.1006-3110.2009.01.016. [22] LIU X, WANG XF, ZHANG T, et al. Clinical analysis of hypotension during hemodialysis[J]. Chin J Blood Purif, 2021, 20(1): 50-53. DOI: 10.3969/j.issn.1671-4091.2021.01.12.刘寻, 王晓菲, 张婷, 等. 血液透析中低血压临床分析[J]. 中国血液净化, 2021, 20(1): 50-53. DOI: 10.3969/j.issn.1671-4091.2021.01.12. [23] TIAN M, ZHA Y, QIE S, et al. Association of body composition and intradialytic hypotension in hemodialysis patients[J]. Blood Purif, 2020, 49(3): 334-340. DOI: 10.1159/000504245. [24] LAUTH M, BERNAL W, DASARATHY S, et al. ESPEN guide-line on clinical nutrition in liver disease[J]. Clin Nutr, 2019, 38(2): 485-521. DOI: 10.1016/j.clnu.2018.12.022. [25] Chinese Society of Hepatology, Chinese society of Gastroenterology, Chinese Medical Association. Clinical guidelines on nutrition in end-stage liver disease[J]. J Clin Hepatol, 2019, 35(6): 1222-1230. DOI: 10.3969/j.issn.1001-5256.2019.06.010.中华医学会肝病学分会, 中华医学会消化病学分会. 终末期肝病临床营养指南[J]. 临床肝胆病杂志, 2019, 35(6): 1222-1230. DOI: 10.3969/j.issn.1001-5256.2019.06.010. [26] EBADI M, BHANJI RA, DUNICHAND-HOEDL AR, et al. Sarcopenia severity based on computed tomography image analysis in patients with cirrhosis[J]. Nutrients, 2020, 12(11): 3463. DOI: 10.3390/nu12113463. [27] GENG N, KONG M, CHEN Y, et al. Value of L3 skeletal muscle index in nutritional diagnosis of end-stage liver disease[J]. J Clin Hepatol, 2021, 37(10): 2493-2496. DOI: 10.3969/j.issn.1001-5256.2021.10.050.耿楠, 孔明, 陈煜, 等. 第三腰椎骨骼肌指数在终末期肝病营养诊断中的应用价值[J]. 临床肝胆病杂志, 2021, 37(10): 2493-2496. DOI: 10.3969/j.issn.1001-5256.2021.10.050. [28] XU M, LI T, KONG M, et al. Psoas muscle index can be used to predict long-term mortality in young male patients with acute-on-chronic liver failure[J]. Front Nutr, 2022, 9: 811826. DOI: 10.3389/fnut.2022.811826. -



 PDF下载 ( 2288 KB)
PDF下载 ( 2288 KB)


 下载:
下载: