再次肝切除术与射频消融治疗亚洲复发性肝细胞癌患者效果比较的Meta分析
DOI: 10.3969/j.issn.1001-5256.2021.05.025
Clinical effect of re-hepatic resection versus radiofrequency ablation in treatment of recurrent hepatocellular carcinoma in Asia: A Meta-analysis
-
摘要:
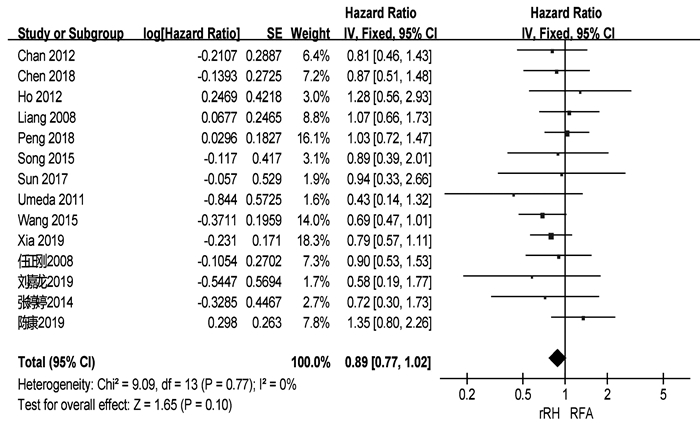
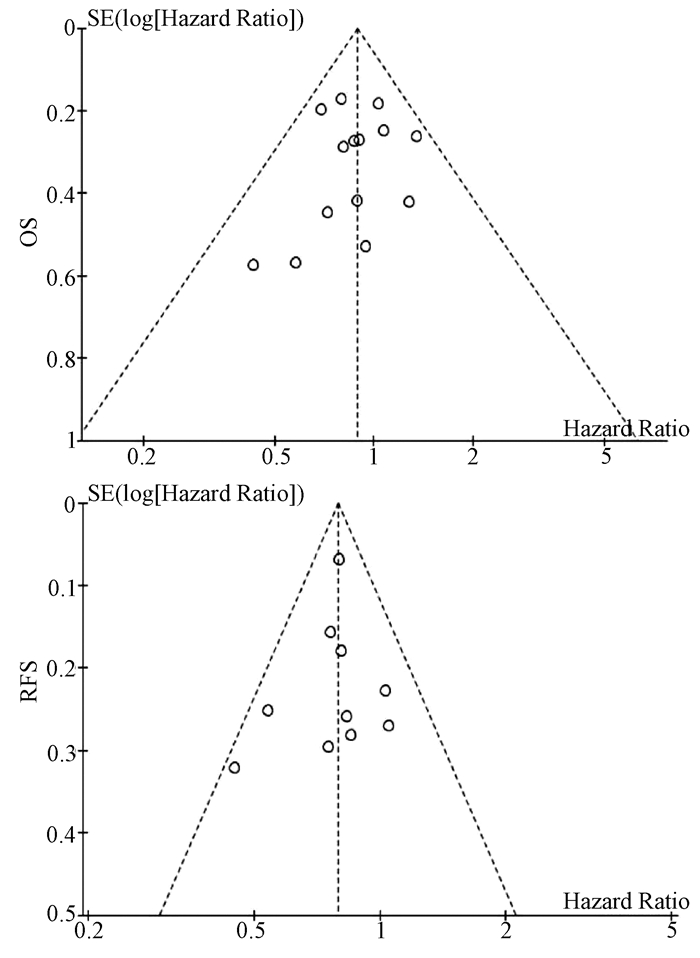
目的 使用Meta分析的方法比较再次肝切除术与射频消融治疗亚洲复发性肝癌患者的安全性与疗效。 方法 系统检索PubMed、中国知网和万方数据库,日期自建库截止至2020年6月15日。由两位评价者独立检索并提取数据,采用RevMan 5.4.1软件进行Meta分析。 结果 共2项随机对照试验和18项回顾性队列研究符合纳入标准,均来自亚洲国家,包含2903例复发性肝癌患者。再次肝切除术组和射频消融组患者围手术期病死率分别为2%和0,围手术期并发症发生率分别为22.4%和3.3%。再次肝切除术组和射频消融组患者术后1、3、5年总生存率分别为92.3%、66.3%、51.1%和91.4%、69.2%、39.9%。两组患者术后1、3、5年无瘤生存率分别为67.9%、48.3%、34.4%和57.5%、27.9%、14.0%。Meta分析结果提示,两组患者的总生存率差异无统计学意义(HR=0.89,95%CI:0.77~1.02,P=0.10),但再次肝切除术组患者的无瘤生存率显著高于射频消融组(HR=0.79,95%CI:0.72~0.87,P<0.001)。 结论 目前证据显示,再次肝切除术治疗复发性肝癌有更高的无瘤生存率,但两组患者的总生存率相似。 -
关键词:
- 癌,肝细胞 /
- 肝切除术 /
- 射频消融 /
- Meta分析(主题)
Abstract:Objective To investigate the safety and efficacy of re-hepatic resection (rHR) versus radiofrequency ablation (RFA) in the treatment of recurrent hepatocellular carcinoma (RHCC) in Asia through a meta-analysis. Methods PubMed, CNKI, and Wanfang Data were searched for related studies published up to June 15, 2020. Two reviewers independently searched for the articles and extracted related data, and RevMan 5.4.1 was used to perform the meta-analysis. Results A total of 2 randomized controlled trials and 18 retrospective cohort studies met the inclusion criteria and involved 2903 patients with RHCC from Asian countries. The mortality rate in the perioperative period was 2% in the rHR group and 0 in the RFA group, and the incidence rate of perioperative complications was 22.4% in the rHR group and 3.3% in the RFA group. The 1-, 3-, and 5-year overall survival rates were 92.3%, 66.3%, and 51.1%, respectively, in the rHR group and 91.4%, 69.2%, and 39.9%, respectively, in the RFA group. The 1-, 3-, and 5-year disease-free survival rates were 67.9%, 48.3%, and 34.4%, respectively, in the rHR group and 57.5%, 27.9%, and 14.0%, respectively, in the RFA group. The Meta-analysis showed that there was no significant difference in overall survival rate between the two groups (hazard ratio [HR]=0.89, 95% confidence interval [CI]: 0.77-1.02, P=0.10), while the rHR group had a significantly higher disease-free survival rate than the RFA group (HR=0.79, 95% CI: 0.72-0.87, P < 0.001). Conclusion Current evidence shows that rHR may help to achieve a higher disease-free survival rate than RFA in the treatment of RHCC, while rHR and RFA have a similar overall survival rate. -
表 1 纳入研究的基线特点
第一作者和年份 国家/地区 纳入时间(年) 组别 样本量 男/女(例) 年龄(岁) 单个/多个肿瘤(例) 复发肿瘤直径(cm) 肝硬化[例(%)] CTP分级(A/B/C,例) 随访(月) Wang 2015[3] 中国 2004—2010 肝切除 128 113/15 50.2±10.1 89/39 2.4±0.9 66(51.6) - - RFA 162 148/14 52.7±10.9 107/55 2.3±0.7 - - - Sun 2017[4] 中国台湾 2002—2014 肝切除 43 34/9 60(35~76) - 1.9(0.8~3.0) 36(83.7) 42/1 53 RFA 57 38/19 63(27~81) - 1.8(1.0~3.0) 50(87.7) 57/0 54 Umeda 2011[5] 日本 1998—2007 肝切除 29 - - - 3.20±0.57 - 29/0 48 RFA 58 - - - 2.1±0.3 - 51/7 48 Song 2015[6] 韩国 1994—2012 肝切除 39 31/8 52.5±9.8 32/7 2.2±1.1 23(59) 39/0 36.3(0.8~126.6) RFA 178 145/33 55.4±10.6 156/22 1.7±0.6 130(73.0) 172/6 44.7(5.6~139.8) Liang 2008[7] 中国 1999—2007 肝切除 44 39/5 48.8±12.0 34/10 ≤3 (26) - 44/0 33.5±24.1 RFA 66 54/12 54.6±10.8 48/18 ≤3 (44) - 64/2 21.1±19.1 Ho 2012[8] 中国台湾 2001—2007 肝切除 54 40/14 56.3±12.3 - 2.9±1.8 26(48.1) 51/2/1 32(0~79) RFA 50 39/11 61.0±11.1 - 2.3±1.9 28(56.0) 50/0 27(0~96) Chan 2012[9] 中国香港 2001—2008 肝切除 29 - 52(38~79) 21/8 2.1(0.8~5.5) 25(86.2) 29/0 44.9 RFA 45 - 59(36~80) 29/16 2.2(0.8~6.0) 40(88.9) 40/5 44.9 Chen 2018[10] 中国 2009—2015 肝切除 48 41/7 73.5±3.5 28/20 2.6±1.1 41(85.4) 39/9 36.9(2~78) RFA 57 51/6 73.7±2.9 30/27 2.5±1.2 49(86.0) 45/12 37.3(2~78) 岑峰2016[11] 中国 2011—2015 肝切除 28 22/6 53.6 12/16 - 23(82.1) 18/10 - RFA 24 19/5 55.7 10/14 - 19(79.2) - - 陈康2019[12] 中国 2005—2014 肝切除 77 65/12 - - - 57(74) 76/1 57(2~168) RFA 82 72/10 - - - 50(61) 77/5 51(4~111) 黄新辉2013[13] 中国 2007—2011 肝切除 66 51/15 50.5±10.1 66/0 2.9±1.1 57(86.3) 66/0 - RFA 46 36/10 54.1±12.1 46/0 2.6±0.9 39(84.8) 46/0 - 梁惠宏2011[14] 中国 1999—2009 肝切除 72 65/7 49±12 72/0 2.1±0.1 - 70/2 36±25 RFA 79 69/10 55±11 79/0 2.5±0.1 - 73/6 32±21 任正刚2008[15] 中国 2000—2005 肝切除 145 127/18 51 127/18 2.0 - 145/0 23(3~88) RFA 68 64/4 52 52/16 2.0 - 68/0 23(3~88) 田正灵2016[16] 中国 2012—2015 肝切除 30 28/2 48.8±9.6 24/6 - 24(80) - 17(6.0~42.5) RFA 27 26/1 50.9±10.1 19/8 - 23(85.2) - 17(6.0~42.5) 张辉2013[17] 中国 2003—2011 肝切除 69 - - - 3.5 61(88.4) 54/15 - RFA 99 - - 2.1 76(76.8) 71/28 - 张婷婷2014[18] 中国 1998—2010 肝切除 27 25/2 47±13 25/2 3.2±1.1 - 27/0 32(9~118) RFA 39 37/2 52±13 37/2 2.7±1.1 - 37/2 28(2~79) Peng 2018[19] 中国 2006—2015 肝切除 79 67/2 55 59/20 ≤3(48) - - 53.2(4~96) RFA 107 95/12 57 75/32 ≤3(73) - - 52.3(3~96) Lu 2020[20] 中国 2004—2015 肝切除 138 124/16 50.1±10.9 112/26 2.8±1.9 96(70) 138/0 37.6 RFA 194 172/22 52.9±11.8 162/32 1.9±0.9 134(69) 194/0 41.6 Xia 2019[21] 中国 2010—2013 肝切除 120 107/13 52.4(25.7~60.5) 96/24 2.9(1.0~5.0) 50(41.7) 120/0 44.3(4.3~90.6) RFA 120 109/11 53.5(28.0~59.9) 94/26 2.7(1.0~4.8) 55(45.8) 120/0 44.3(4.3~90.6) 刘嘉龙2019[22] 中国 2016—2017 肝切除 39 38/1 50.0±10.0 37/2 2.1±0.7 37(94.9) 38/1 24 RFA 41 37/4 48.9±11.3 39/2 1.8±0.8 39(95.1) 39/2 24 注:-,未报道。 表 2 纳入患者的治疗结局
第一作者和年份 组别 并发症发生率(%) 围手术期病死率(%) 复发[例(%)] RFS OS 1年 3年 5年 P值1) 1年 3年 5年 P值1) Wang 2015[3] 肝切除 - - - - - - - 97.7 84.1 64.5 <0.001 RFA - - - - - - 96.9 73.4 37.0 Sun 2017[4] 肝切除 16 2 30(69.8) 57.0 32.1 28.6 0.89 97.6 82.7 56.4 0.69 RFA 7 0 41(71.9) 60.8 26.6 16.6 98.2 77.2 52.6 Umeda 2011[5] 肝切除 - - - - - - - 93.1 66.8 58.1 0.899 RFA - - - - - - 94.7 75.1 48.3 Song 2015[6] 肝切除 64 2.6 18(46.2) 66.1 48.5 43.1 0.834 88.8 88.8 83.9 0.686 RFA 2.2 0 117(65.7) 70.1 40.8 30.0 98.9 82.5 71.0 Liang 2008[7] 肝切除 68.2 0 86.4 - - - - 78.6 44.5 27.6 0.79 RFA 3.0 0 78.8 - - - 76.6 48.6 39.9 Ho 2012[8] 肝切除 - - - - - - - - - 72.0 - RFA - - - - - - - - 83.0 Chan 2012[9] 肝切除 24.1 0 21(72.4) 41.1 24.2 24.2 0.14 89.7 56.5 35.2 0.51 RFA 2.2 2.2 38(84.4) 32.2 12.4 9.3 83.7 43.1 29.1 Chen 2018[10] 肝切除 25 2.1 26(54.2) 73.1 49.7 40.7 0.465 76.3 52.5 42.6 0.413 RFA 0 0 27(47.4) 69.5 37.8 33.1 78.2 40.8 36.7 岑峰2016[11] 肝切除 50 0 - 46.4 0 0 - - - - - RFA - 0 - 20.8 0 0 - - - 陈康2019[12] 肝切除 17.1 1.3 - - - - - 88.8 68.8 51.1 0.258 RFA 9.8 0 - - - - 91.4 73.4 61.1 黄新辉2013[13] 肝切除 18.1 0 - 43.9 14.4 8.2 0.548 89.5 54.3 28.8 0.780 RFA 0 0 - 56.9 12.4 5.0 82.6 50.8 20.5 梁惠宏2011[14] 肝切除 36 0 ≤1年: 39>1年: 33 - - - - 95.3 65.7 54.5 >0.05 RFA 13 0 ≤1年: 37>1年: 42 - - - - 100 79.4 62.1 任正刚2008[15] 肝切除 5.5 0 ≤2年: 71>2年: 74 79.4 48.1 34.4 0.001 88.1 62.6 41.0 0.693 RFA 1.5 0 ≤2年: 37>2年: 31 58.0 27.8 12.4 94.7 65.1 37.3 田正灵2016[16] 肝切除 6.7 0 10(33.3) 73.3 64.3 - 0.002 96.7 93.3 - 0.54 RFA 3.7 0 24(88.9) 46.7 26.7 - 96.3 84.0 - 张辉2013[17] 肝切除 15.9 1.45 - - - - - 68.2 45.4 - >0.05 RFA 0 0 - - - - 73.7 53.6 - 张婷婷2014[18] 肝切除 - 0 22(56.4) 66.7 50.7 43.4 0.323 96.2 76.9 61.2 0.471 RFA - 0 14(52.9) 65.8 28.0 14.0 86.2 73.3 62.2 Peng 2018[19] 肝切除 17.7 1.3 - 64.8 41.6 38.3 0.258 84.8 60.2 51.9 0.871 RFA 4.7 0 - 58.2 35.2 29.6 84.6 66.9 49.1 Lu 2020[20] 肝切除 - - - 91.8 82.0 72.9 0.38 - - - - RFA - - - 94.4 75.4 61.7 - - - Xia 2019[21] 肝切除 22.4 0 60.8 85.0 52.4 36.2 0.09 92.5 65.8 43.6 0.17 RFA 7.3 0 64.2 74.2 41.7 30.2 87.5 52.5 38.5 刘嘉龙2019[22] 肝切除 35.9 0 19(48.7) 69.2 - - <0.001 92.3 - - 0.292 RFA 4.9 0 32(78.0) 26.8 - - 85.4 - - 注:-,未报道;1) P值来源于原文报道。 -
[1] WANG YY, LIU JM, WANG LJ, et al. Prognostic value of tumor burden score in patients with hepatocellular carcinoma[J]. Chin J Oncol Prev Treat, 2019, 11(5): 393-397. DOI: 10.3969/j.issn.1674-5671.2019.05.06.王言焱, 刘佳明, 王立军, 等. 肿瘤负荷评分在肝细胞癌患者预后预测中的价值[J]. 中国癌症防治杂志, 2019, 11(5): 393-397. DOI: 10.3969/j.issn.1674-5671.2019.05.06. [2] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma[J]. J Hepatol, 2018, 69(1): 182-236. DOI: 10.1016/j.jhep.2018.03.019. [3] WANG K, LIU G, LI J, et al. Early intrahepatic recurrence of hepatocellular carcinoma after hepatectomy treated with re-hepatectomy, ablation or chemoembolization: A prospective cohort study[J]. Eur J Surg Oncol, 2015, 41(2): 236-242. DOI: 10.1016/j.ejso.2014.11.002. [4] SUN WC, CHEN IS, LIANG HL, et al. Comparison of repeated surgical resection and radiofrequency ablation for small recurrent hepatocellular carcinoma after primary resection[J]. Oncotarget, 2017, 8(61): 104571-104581. DOI: 10.18632/oncotarget.21604. [5] UMEDA Y, MATSUDA H, SADAMORI H, et al. A prognostic model and treatment strategy for intrahepatic recurrence of hepatocellular carcinoma after curative resection[J]. World J Surg, 2011, 35(1): 170-177. DOI: 10.1007/s00268-010-0794-8. [6] SONG KD, LIM HK, RHIM H, et al. Repeated hepatic resection versus radiofrequency ablation for recurrent hepatocellular carcinoma after hepatic resection: A propensity score matching study[J]. Radiology, 2015, 275(2): 599-608. DOI: 10.1148/radiol.14141568. [7] LIANG HH, CHEN MS, PENG ZW, et al. Percutaneous radiofrequency ablation versus repeat hepatectomy for recurrent hepatocellular carcinoma: A retrospective study[J]. Ann Surg Oncol, 2008, 15(12): 3484-3493. DOI: 10.1245/s10434-008-0076-y. [8] HO CM, LEE PH, SHAU WY, et al. Survival in patients with recurrent hepatocellular carcinoma after primary hepatectomy: Comparative effectiveness of treatment modalities[J]. Surgery, 2012, 151(5): 700-709. DOI: 10.1016/j.surg.2011.12.015. [9] CHAN AC, POON RT, CHEUNG TT, et al. Survival analysis of re-resection versus radiofrequency ablation for intrahepatic recurrence after hepatectomy for hepatocellular carcinoma[J]. World J Surg, 2012, 36(1): 151-156. DOI: 10.1007/s00268-011-1323-0. [10] CHEN S, PENG Z, XIAO H, et al. Combined radiofrequency ablation and ethanol injection versus repeat hepatectomy for elderly patients with recurrent hepatocellular carcinoma after initial hepatic surgery[J]. Int J Hyperthermia, 2018, 34(7): 1029-1037. DOI: 10.1080/02656736.2017.1387941. [11] CEN F. Analysis of curative effect of repeated hepatectomy for recurrent HCC[D]. Hangzhou: Zhejiang University School of Medicine, 2016.岑峰. 复发性肝癌行再次肝切除术治疗的疗效分析研究[D]. 杭州: 浙江大学, 2016. [12] CHEN K, LIU XY, TENG YX, et al. Rehepatectomyand radiofrequency ablation for patients with recurrent hepatocellular carcinoma[J]. Chin J Practic Surg, 2019, 39(10): 1060-1064. DOI: 10.19538/j.cjps.issn1005-2208.2019.10.16.陈康, 刘新宇, 滕煜宪, 等. 再次肝切除与射频消融治疗复发性肝癌疗效对比研究[J]. 中国实用外科杂志, 2019, 39(10): 1060-1064. DOI: 10.19538/j.cjps.issn1005-2208.2019.10.16. [13] HUANG XH, HUANG Y, LIN KC, et al. The curative efficacy comparison of percntaneons radiofrequency ablation versus surgical re-resection for recurrent small hepatocellular carcinoma[J]. J Abdominal Surg, 2013, 26(2): 93-95. DOI: 10.3969/j.issn.1003-5591.2013. 02.008.黄新辉, 黄尧, 林科灿, 等. 复发性小肝细胞癌射频消融与再手术切除疗效的分析[J]. 腹部外科, 2013, 26(2): 93-95. DOI: 10.3969/j.issn.1003-5591.2013. 02.008. [14] LIANG HH, PENG ZW, CHEN MS, et al. Effects of percutaneous radiofrequency ablation and repeat hepatectomy for the treatment of solitary recurrent hepatocelluar carcinoma with the diameter no more than 3 cm[J]. Chin J Dig Surg, 2011, 10(1): 36-39. DOI: 10.3760/cma.j.issn. 1673-9752. 2011.01.010.梁惠宏, 彭振维, 陈敏山, 等. 经皮射频消融与再手术治疗单个直径≤3 cm的复发性肝癌的疗效比较[J]. 中华消化外科杂志, 2011, 10(1): 36-39. DOI: 10.3760/cma.j.issn.1673-9752. 2011.01.010. [15] REN ZG, GAN YH, FAN J, et al. Treatment of postoperative recurrence of hepatocellular carcinoma with radiofrequency ablation comparing with repeated surgical resection[J]. Chin J Surg, 2008, 46(21): 1614-1616. DOI: 10.3321/j.issn:0529-5815.2008.21.005.任正刚, 干育红, 樊嘉, 等. 射频毁损术与再手术切除治疗复发性小肝癌对照研究[J]. 中华外科杂志, 2008, 46(21): 1614-1616. DOI: 10.3321/j.issn:0529-5815.2008.21.005. [16] TIAN ZL. Investigate the efficacy between radiofrequency ablation and surgical resection in the treatment of small recurrent hepatocellular carcinoma: An retrospective analysis of 57 cases[D]. Nanning: Guangxi Medical University, 2016.田正灵. 射频消融与手术切除治疗复发性小肝细胞性肝癌的疗效比较分析(附57例病例分析)[D]. 南宁: 广西医科大学, 2016. [17] ZHANG H, XU XB, HE XJ, et al. Compare of the efficacy between re-operative and radiofrequency ablation on postoperative recurrent carcinoma[J]. Med J West China, 2013, 25(12): 1816-1818. DOI: 10.3969/j.issn.1672-3511.2013.12.019.张辉, 徐新保, 何晓军, 等. 原发性肝癌术后复发再手术切除与射频消融治疗的疗效比较[J]. 西部医学, 2013, 25(12): 1816-1818. DOI: 10.3969/j.issn.1672-3511.2013.12.019. [18] ZHANG TT, LI KY, LUO HC, et al. Long-term outcomes of percutaneous microwave ablation versus repeat hepatectomy for treatment of late recurrent small hepatocellular carcinoma: A retrospective study[J]. Natl Med J China, 2014, 94(33): 2570-2572. DOI: 10.3760/cma. j.issn.0376-2491.2014.33.004.张婷婷, 李开艳, 罗鸿昌, 等. 经皮微波消融和二次手术治疗晚期复发型小肝癌的长期疗效观察[J]. 中华医学杂志, 2014, 94(33): 2570-2572. DOI: 10.3760/cma.j.issn.0376-2491. 2014.33.004. [19] PENG Z, WEI M, CHEN S, et al. Combined transcatheter arterial chemoembolization and radiofrequency ablation versus hepatectomy for recurrent hepatocellular carcinoma after initial surgery: A propensity score matching study[J]. Eur Radiol, 2018, 28(8): 3522-3531. DOI: 10.1007/s00330-017-5166-4. [20] LU LH, MEI J, KAN A, et al. Treatment optimization for recurrent hepatocellular carcinoma: Repeat hepatic resection versus radiofrequency ablation[J]. Cancer Med, 2020, 9(9): 2997-3005. DOI: 10.1002/cam4.2951. [21] XIA Y, LI J, LIU G, et al. Long-term effects of repeat hepatectomy vs percutaneous radiofrequency ablation among patients with recurrent hepatocellular carcinoma: A randomized clinical trial[J]. JAMA Oncol, 2020, 6(2): 255-263. DOI: 10.1001/jamaoncol.2019.4477. [22] LIU JL, HUANG D, CAO L, et al. Laparoscopic hepatectomy versus radiofrequency ablation in treatment of recurrent hepatocellular carcinoma: A prospective randomized control study based on interim follow-up analysis[J]. J Third Milit Med Univ, 2019, 41(5): 467-472. DOI: 10.16016/j.1000-5404.201811005.刘嘉龙, 黄登, 曹利, 等. 腹腔镜肝切除术和射频消融术治疗复发性肝癌的前瞻性随机对照研究(中期随访分析)[J]. 第三军医大学学报, 2019, 41(5): 467-472. DOI: 10.16016/j.1000-5404.201811005. [23] CHAN AC, CHAN SC, CHOK KS, et al. Treatment strategy for recurrent hepatocellular carcinoma: Salvage transplantation, repeated resection, or radiofrequency ablation?[J]. Liver Transpl, 2013, 19(4): 411-419. DOI: 10.1002/lt.23605. [24] CHEN R, GAN Y, GE N, et al. Transarterial chemoembolization versus radiofrequency ablation for recurrent hepatocellular carcinoma after resection within barcelona clinic liver cancer stage 0/A: A retrospective comparative study[J]. J Vasc Interv Radiol, 2016, 27(12): 1829-1836. DOI: 10.1016/j.jvir.2016.06.010. [25] HIROKAWA F, HAYASHI M, MIYAMOTO Y, et al. Appropriate treatment strategy for intrahepatic recurrence after curative hepatectomy for hepatocellular carcinoma[J]. J Gastrointest Surg, 2011, 15(7): 1182-1187. DOI: 10.1007/s11605-011-1484-z. [26] WANG N, ZHENG JL, JIANG L. Clinical effect of surgical resection versus radiofrequency ablation in treatment of multiple liver cancer in different liver segments meeting the Milan criteria[J]. J Clin Hepatol, 2020, 36(4): 792-797. DOI: 10.3969/j.issn.1001-5256.2020.04.017.王宁, 郑金利, 蒋利. 手术切除与射频消融治疗符合米兰标准的不同肝段多发肝癌的效果分析[J]. 临床肝胆病杂志, 2020, 36(4): 792-797. DOI: 10.3969/j.issn.1001-5256.2020.04.017. [27] DUAN C, LIU M, ZHANG Z, et al. Radiofrequency ablation versus hepatic resection for the treatment of early-stage hepatocellular carcinoma meeting Milan criteria: A systematic review and meta-analysis[J]. World J Surg Oncol, 2013, 11(1): 190. DOI: 10.1186/1477-7819-11-190. [28] LIN SM, LIN CJ, LIN CC, et al. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less[J]. Gut, 2005, 54(8): 1151-1156. DOI: 10.1136/gut.2004.045203. [29] PENG ZW, ZHANG YJ, CHEN MS, et al. Risk factors of survival after percutaneous radiofrequency ablation of hepatocellular carcinoma[J]. Surg Oncol, 2008, 17(1): 23-31. DOI: 10.1016/j.suronc.2007.08.002. [30] LIVRAGHI T, LAZZARONI S, MELONI F. Radiofrequency thermal ablation of hepatocellular carcinoma[J]. Eur J Ultrasound, 2001, 13(2): 159-166. DOI: 10.1016/s0929- 8266(01)00128-8. [31] HUANG J, YAN L, CHENG Z, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria[J]. Ann Surg, 2010, 252(6): 903-912. DOI: 10.1097/SLA.0b013e3181efc656. [32] ZHONG JH, KE Y, GONG WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma[J]. Ann Surg, 2014, 260(2): 329-340. DOI: 10.1097/SLA.0000000000000236. [33] LEE S, KANG TW, SONG KD, et al. Effect of microvascular invasion risk on early recurrence of hepatocellular carcinoma after surgery and radiofrequency ablation[J]. Ann Surg, 2019, 273(3): 564-571. DOI: 10.1097/SLA.0000000000003268. -



 PDF下载 ( 2595 KB)
PDF下载 ( 2595 KB)


 下载:
下载: